. This is really very promising. It has taken a vast amount of time, but all that work allows rapid resolution for the ones locked out. This means that we have not stood still and that the whole armory will enter the pharmacopia to be rigorously applied for the benefit of mental health and also mental development.
The military has been doing all this in secret but we may now find the doors opening up.
all good news for the patient.
Medical Researchers Are Steps From Legalizing Ecstasy. Here's How They Did It.
Reason Staff|Jul. 18, 2017 8:31 am
Joanna AndreassonIn a new online feature, Mike Riggs looks at the decades-long effort to legalize MDMA and other psychedelic drugs for medical use:
http://reason.com/blog/2017/07/18/new-at-reason-medical-researchers-are-st
In January 1967, roughly 20,000 young people gathered at Golden Gate Park for the Human Be-In, a kind of outdoor conference for hippie counterculture. The event introduced the word "psychedelic" to the American mainstream, and the psychedelic evangelist Timothy Leary to San Francisco.
California and Nevada had banned LSD a year earlier, following New York, which banned it in 1965. Leary, a psychologist who'd recently been canned from his faculty gig at Harvard for sharing psychedelic drugs with undergraduates, believed there was no longer any point in negotiating with the powers that be. His message was blunt: "Drop out of high school, drop out of college, drop out of graduate school."
The Man—mostly government, but also society and authority figures of all kinds—was attempting to eradicate psychedelic drugs and the liberation they bestowed. That required a proportionately rebellious response: "Turn on, tune in, drop out." Students around the country heard Leary's words, and many did as he exhorted. The Man heard him, too, and doubled down on its efforts to bury the psychedelic drug era under a mound of criminal sanctions and red tape. Within a few years, psychedelic drugs were completely regulated out of recreational settings, then therapeutic settings, and finally research settings.
Fifty years and a few months later, at a Marriott hotel 14 miles from Golden Gate Park, the Multidisciplinary Association for Psychedelic Studies (MAPS) hosted nearly 3,000 researchers, students, and enthusiasts for Psychedelic Science 2017, a six-day conference on what's being done to turn illegal psychedelic drugs into legal pharmaceutical products. Once again, the avatars of psychedelic culture had gathered to compare notes, share their experiences, and talk strategy.
This time, the message was different: Stay in school. Apply for research grants. Design clinical trials. Show your work. Evangelize, yes, but with a new audience in mind—not the counterculture, but the Man himself.
"Regulators, governments, health economists, health systems, insurers, health-care professionals, and—most importantly—patients," said George Goldsmith, the former CEO of McKinsey & Company's TomorrowLab, and an advocate for the kind of therapeutic innovation psychedelic researchers are hoping to achieve. "That's the next community that actually needs to be engaged here."
Sitting onstage next to Goldsmith was Thomas Insel, a psychiatrist and former director of the National Institute of Mental Health. Insel, who's spent a lot of time in recent years bemoaning the paucity of effective psychiatric drugs, was blunter still. "I would encourage you to be more Catholic than the Pope. You've got to be more rigorous than the people working in the pharmaceutical industry studying more traditional compounds that aren't controlled [substances]." One adverse patient reaction for which clinical investigators were not prepared, he argued, could "poison the well."
"I know you don't want to hear that," he added. "But it's really easy to mess things up."Today's psychedelic drug community is fiercely committed to avoiding a repeat of the 1960s' culture wars, in no small part because their tie-dyed predecessors lost. Insel and Goldsmith, while not psychedelic researchers themselves, reflect the current movement's willingness to work with more staid actors in the field of medicine.
At the Human Be-In, where Leary delivered his fiery exhortation, Hell's Angels provided security and attendees openly blazed and tripped. At Psychedelic Science 2017, a printed program encouraged those of us in attendance to "respect the work that happens within legal regulatory systems" by limiting our "engagement with psychedelic and other illegal drugs to the realm of intellectual discussion."
The contemporary movement even looks different. At the height of his fame, Leary, who passed away in 1996, dressed like a hippie priest, in flowing robes and mystical pendants. Rick Doblin, the president and founder of MAPS and the de facto leader of psychedelic drug research in the U.S., dresses like a bank manager: dark suit, dark shoes, muted tie.
Rather than fleeing academia—or being forced out, as Leary was—psychedelic researchers are burrowing in, with appointments at Stanford, the University of California, Johns Hopkins, New York University, Imperial College London, and dozens of other respected institutions around the world.
The maturation of the field is not nearly as remarkable as the medical utility researchers are beginning to uncover, but the latter is the result of the former. The world lost a generation's worth of promising research and medical discovery following the tumult of the 1960s. For more than 30 years, Doblin and a small band of experts and professionals have worked to overcome the bureaucratic and scientific barriers to safe and legal access.
They've donned suits, worked with the Food and Drug Administration (FDA), and discouraged the kind of recreational use that came to define the 1960s. They turned on and tuned in to the legitimizing structures that Leary and his cohort rejected—and it has worked. In May of this year, the FDA approved yet another protocol from MAPS for its clinical trial of MDMA-assisted psychotherapy. They are leading a peaceful and methodical revolution in the way scientists, doctors, and government officials talk and think about psychedelics. As soon as 2021, some of these drugs could be legal medicine.
The Pharmaceutical Origins of Pyschedelic Drugs

Albert
Hofmann at an event in Switzerland commemorating the 50th anniversary
of his discover of LSD. PHOTO CREDIT: Philip H. BaileyLSD-25—the
psychoactive substance we now simply know as LSD, or "acid"—was first
synthesized in 1938 by the chemist Albert Hofmann at Sandoz
Pharmaceuticals in Switzerland.
Hofmann first tested the compound, made from the fungus ergot, in
animals as a circulatory and respiratory stimulant. Initially, it
"aroused no special interest" in Sandoz's medical team, according to
Hofmann's memoir, LSD: My Problem Child. Five years later,
while working with the compound again, Hofmann accidentally consumed
some and experienced "a not unpleasant intoxicated-like condition,
characterized by an extremely stimulated imagination."
In the 1950s, LSD, along with other psychoactive drugs, such as
mescaline and psilocybin, which come from peyote and mushrooms,
respectively, gained a following among European and North American
psychiatrists, who saw therapeutic value in their capacity for disarming
and unlocking the mind. They gave LSD to trauma victims and to
alcoholics. In conjunction with psychotherapy, they reported promising
results.
Psychedelic drugs reached the American mainstream in the late 1950s,
thanks to a series of captivating articles in national publications.
Today's psychedelic drug community is
fiercely committed to avoiding a repeat of the 1960s culture wars, in no
small part because their tie-dyed predecessors lost.
The first was Gordon Wasson's 1957 story in Life, "Seeking
the Magic Mushroom: a New York banker goes to Mexico's mountains to
participate in the age old rituals of Indians who chew strange growths
that produce visions." Then, in 1959, Look published "The
Curious Story Behind the New Cary Grant," in which the actor revealed
that nothing he'd done for his mental health helped him as much as using
LSD under the guidance of a psychoanalyst. A few years later, two
separate books about LSD-assisted therapy—1961's Exploring Inner Space, by Jane Dunlap, and 1962's My Self and I, by Thelma Moss (under the pen name Constance Newland)—hit the bestseller list. In LSD: My Problem Child,
Hofmann writes that the sudden media onslaught "led to broad diffusion
of self-experimentation with the new drug." LSD was having its moment.
Yet as the 1960s crescendoed toward a manic conclusion, clinicians
watched helplessly as a thousand converging phenomena earned them and
their long-haired fellow travelers a brutal rebuke. Hofmann notes that
as LSD use spread, so did the phenomenon of the "horror trip." States
moved quickly to ban LSD, and in 1967, the National Institute of Mental
Health halted all of its in-house psychedelic studies and yanked funding
from outside researchers.
The Manson Family murders in 1969 provided further justification for
the panic. While Charles Manson's history of antisocial and pathological
violence predated his use of LSD by at least two decades, news reports
described him and his followers as acid-dropping hippies. Psychedelics
were guilty by association. Washington turned the final screw in 1970,
passing the Controlled Substances Act and installing the Justice
Department as a gatekeeper for Schedule I drug research.
Yet what could have been the end for psychedelics instead laid the
groundwork for a transformation.
Rather than going away, they went
underground.
Rick Doblin and the Path to Medical Research
Before Rick Doblin steps onstage at Psychedelic Science 2017, an old
photo of him appears onscreen. He is 18 or so, shirtless, lithe, and
smirking. Curly tresses frame his face. It was not Doblin's idea to show
this picture, and he guffaws as he takes the stage and begins his
presentation: a brief history of the psychedelic research movement.
Although his presentation starts in the '70s, understanding the
current moment begins earlier, with Doblin's own life, and Doblin's
personal transition from post-war babe to hippie rebel.
Born in 1953 to upper-middle-class Jewish parents in suburban
Illinois, he first discovered psychedelia as a high schooler, via a copy
of Ken Kesey's One Flew Over the Cuckoo's Nest. After a brief
flirtation with Barry Goldwater's brand of conservatism, he veered
leftward, volunteering for the presidential campaign of progressive
darling Eugene McCarthy in 1968 and refusing to register for the
Selective Service. When it came time to pick a college, he chose New
College of Florida, a crunchy liberal enclave near Tampa Bay that had
existed for only a decade.
Doblin was not at ease in his own body or mind. Then, at New College,
he tried LSD for the first time. The experience was a revelation: "He
had made himself who he was," writes Tom Schroder in Acid Test: LSD, Ecstasy, and the Power to Heal. "With the assistance of the LSD experience, he could change."
New College was inundated with psychedelic drugs, and Doblin fell in
love: with LSD, with mescaline, with the way the drugs opened him up to
himself and to the world. Like Leary, he wanted to proselytize. But the
drug's Schedule I status—reserved for substances the government had
deemed highly addictive, potentially dangerous, and therapeutically
useless—would limit what he or anyone else could do to expand access.
This was not yet true, however, of MDMA, which Doblin learned about in 1982 at the Esalen Institute in Big Sur, California, and tried for the first time that October.
"It was phenomenal," Doblin told Schroder. "It was clearer and didn't affect the perceptions the way psychedelics did."
The technical name for MDMA is 3,4-Methylenedioxymethamphetamine, but
most recreational users know it as "molly" or "ecstasy." The drug was
created by Merck Pharmaceutical in the early 1900s. It wasn't designed
for any particular medical ailment, and like LSD at Sandoz, initially
failed to elicit interest from Merck's clinical researchers.
 \
\
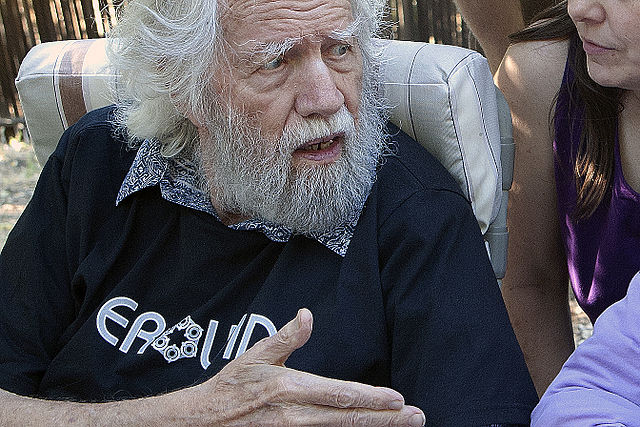
AlexanderThen,
in the 1970s, psychedelic chemist Alexander Shulgin, a veteran of Dow
Chemical, re-synthesized it and began self-experimenting. Shulgin, who
died in 2014 at the age of 89, has since become recognized among
psychedelic researchers and enthusiasts as the movement's chemical
godfather. Educated at Harvard and Berkley, he synthesized hundreds of
compounds and tested all of them on himself. MDMA struck a chord with
him, and he became its first proponent as a next-generation psychiatric
tool.
Shulgin's promotion of MDMA gave it immediate credibility among
therapists and recreational users alike. Psychiatrists who had been
forced to end human trials with LSD were able to resume their work with
MDMA, then largely unknown to federal regulators and law enforcement.
Unlike LSD trips, which can drastically distort the user's
perception, MDMA is far more forgiving psychologically. It's a mood
booster, active for a relatively short amount of time—three or four
hours, rather than LSD's eight to 12—and it doesn't cause
hallucinations. Its amphetamine content, meanwhile, makes it a powerful
stimulant. In short, MDMA makes users feel happy, talkative, energetic,
and sensitive to stimuli, but it causes very little of the cognitive
instability inherent to more classical hallucinogens like mescaline,
psilocybin, and LSD.
Of all the psychedelic drugs, none is currently closer to achieving
regulatory legitimacy than MDMA. And the reason is that Doblin has spent
the better part of three decades working within the confines of the
federal drug bureaucracy.
Early Setbacks With the DEA
Eventually, Doblin's presentation at Psychedelic Science 2017 arrives
at the year 1984. This was when the Drug Enforcement Administration
(DEA) published a noticed in the Federal Register announcing its
intention to add MDMA to Schedule I of the Controlled Substances Act,
making it illegal to manufacture, sell, buy, or prescribe it.
The DEA announcement came at the behest of Democratic Texas Sen.
Lloyd Bentsen, whose state had become ground zero for recreational MDMA
use. In Texas and elsewhere, it had become a popular nightclub drug, and
clubgoers consumed large doses along with alcohol, leading to emergency
department admissions for dehydration and amphetamine psychosis. As
media outlets got wind of a novel substance that fueled all-night
parties and sent people to the hospital, so did the Drug Enforcement
Administration. Doblin's fight against the DEA's move would set the
course for his professional future.
At the conference, another picture of Doblin appears onscreen. He is
in front of the DEA's headquarters, wearing a dress shirt tucked into
jeans, preparing to step inside and deliver a petition calling for an
administrative law judge hearing to contest MDMA's scheduling.
"Rick thought he could just kick the door down," David Nichols tells
me by phone. Nichols collaborated with Shulgin, but now that Shulgin is
gone, he is the world's foremost authority on psychedelic chemistry.
Since 1969, he has developed roughly 150 different psychedelic molecules
and held academic appointments at Purdue, the University of North
Carolina at Chapel Hill, and the University of Indiana Medical School.
As the DEA was preparing to ban MDMA, he worked with Doblin to brew a
batch of the drug that could be used for research.
Doblin's door-kicking almost worked.
Even before the DEA announced its plan, Doblin had joined forces with
a bevy of psychotherapists who wanted to protect their new therapeutic
tool. Among them was George Greer, a psychiatrist in Santa Fe, New
Mexico, who worked in private practice and with drug-addicted inmates at
the Penitentiary of New Mexico.
In a 1984 letter
to the DEA requesting a scheduling hearing, Greer said he had
administered MDMA safely to his patients and referred the agency to his
peer-reviewed research "describing the useful and beneficial effects of
MDMA when used under medical supervision." Other therapists also wrote to the DEA about their work with MDMA-assisted psychotherapy. According to Richard Boire of the Center for Cognitive Liberty and Ethics, "Not one person wrote to support the DEA's intention to place MDMA in Schedule I."
The backlash to the scheduling announcement, and the petition Doblin
submitted, led to a series of nine hearings before a DEA administrative
law judge named Francis Young in 1985. At the same time, Doblin was
working to get stories about MDMA-assisted psychotherapy into the press,
convinced that a doing so would force the DEA to put it into Schedule
III, which would make it a prescription drug.
At first, the strategy showed promise. Hearings featured compelling
testimony from medical doctors and their patients in favor of
prescription status for MDMA, and media reports painted the DEA as
overzealous in its efforts.
Then in the spring of 1985, daytime TV host Phil Donahue convened a
panel of experts to debate MDMA on his show. During that fateful taping,
University of Chicago psychiatrist Charles Schuster, who had founded
the school's Drug Abuse Research Center, announced his suspicion that
MDMA was likely neurotoxic and capable of causing brain damage. A DEA
representative named Gene Haislep was also on the panel.
Not long after the episode aired, on July 1, 1985, the DEA declared
it would use emergency powers to force MDMA into Schedule I on an
expedited basis. The cruel irony of Schuster's missive: According to Acid Test, Doblin had recommended Donahue include him on the panel.
A year after the emergency scheduling, Young, the DEA administrative
law judge, ruled that the DEA had made a mistake and that MDMA should be
placed in Schedule III. "The overwhelming weight of medical opinion
evidence received in this proceeding concurred that sufficient
information on MDMA existed to support a judgment by reputable
physicians that MDMA was safe to use under medical supervision," Young wrote in his opinion. "No evidence was produced of any instances where MDMA was used in therapy with less than wholly acceptable safety."
The odd thing about the role of the DEA's administrative law judges
is that their opinions are completely advisory. The agency decided to
ignore Young's. Several legal challenges ensued, but by 1988, the DEA
had won. MDMA was a Schedule I drug.
Fighting that scheduling initially seemed easy: Doblin and his allies
knew the drug could help people, Young had ruled in their favor, and
major newspapers and magazines across the U.S. had run positive stories
from psychiatrists and their patients discouraging a federal crackdown.
"No evidence was produced of any instances
where MDMA was used in therapy with less than wholly acceptable safety,"
wrote the DEA administrative law judge.
But moving it out of Schedule I has been arduous. The average cost of
taking a central nervous system drug through stage two and three
clinical trials—the only way to get MDMA rescheduled—is tens of millions
of dollars. When Greer first wrote to the DEA, he said a pharmaceutical
company had quoted him a price of $40 to $80 million. Today, MAPS
expects phase-three trials for MDMA-assisted psychotherapy for PTSD to
cost between $20 and $25 million. "However," Doblin notes, "we have
spent many millions already getting to this point."
Cost aside, the goal was unprecedented: No drug has been moved from
Schedule I to prescription status since the Controlled Substances Act
passed in 1970.
But working within the system—the idea that Leary had rebelled
against—was now the only option. So in 1986, Doblin founded MAPS in
hopes of raising money for the clinical trials. There were two things he
needed that money couldn't buy: a receptive audience at the Food and
Drug Administration (FDA), which hadn't approved psychedelic research
with human subjects in nearly two decades, and a credentialed researcher
willing to stick his neck out for MDMA.
The FDA Makes a Critical Turn
In 1989, after two decades of just saying "no" to psychedelic
researchers, a change at the FDA gave Doblin his receptive audience.
That year, the agency launched something called the Pilot Drug
Evaluation Staff. An incubator for ways to speed up and simplify drug
approval, Pilot Drug was put it in charge of reviewing Investigational
New Drug (IND) applications for Schedule I substances.
The IND application is the first step in creating a legal drug.
Without it, researchers can't receive illegal substances across state
lines or move trials from animals to humans. Successful IND applications
require sponsors to provide detailed explanations of toxicology and
pharmacology in animals, as well as any human data available from
studies conducted overseas.
"We went back through every single Investigative New Drug (IND)
application that was still active, but on Clinical Hold," Pilot Drug
medical officer Curtis Wright told reporter Cheryl Pellerin, author of
1998's Trips: How Hallucinogens Work in Your Brain. "And we
started calling people. We found requests for hallucinogen research,
marijuana research, LSD research, undercapitalized venture-capital drug
products—all kinds of things. But many were put on hold, and no one had
figured out how to break them free."
The Pilot Drug team restored legitimacy to psychedelic research. In
1990, the division approved a proposal by Rick Strassman at the
University of New Mexico to study the effect on human subjects of DMT, a
short-acting hallucinogen found in various plants. In 1991, Pilot Drug
approved neuropsychopharmacologist Albert Kurland's request to
investigate LSD-assisted psychotherapy. (Kurland failed to raise the
necessary funds, and the study never took place.)
But Doblin still needed someone who could run a trial for MDMA.
Shulgin, the chemist who'd rescued MDMA from the dustbin, had someone in
mind: Charles Grob, then a psychiatrist and medical faculty member at
the University of California, Irvine.
"Rick and I met in 1990, after I published a letter to the editor in the Archives of General Psychiatry
critiquing a very flawed study report from Johns Hopkins alleging that
MDMA caused 'neurotoxicity,'" Grob says. "I described in my letter to
the editor that the investigators used a flawed methodology,
misinterpreted their data, and presented conclusions that could not hold
up to the facts."
Shulgin sent Grob's letter to Doblin, and Doblin asked Grob in 1990
if he wanted to run a MAPS-sponsored clinical trial on the therapeutic
potential of MDMA. "I replied if there were adequate funding I would be
very interested to conduct such a study," Grob says.
In 1992, Grob, currently a psychiatrist at Harbor–UCLA Medical
Center, submitted a protocol to the FDA for investigating MDMA-assisted
psychotherapy in terminally ill cancer patients. It would be the biggest
test yet of the FDA's commitment to letting science, rather than drug
war agitprop, guide the regulatory process.
The FDA commenced its review and asked the National Institute on Drug
Abuse to do the same. Psychedelic researchers were invited to testify
before both agencies in the summer of 1992. Among them were Grob,
Doblin, Nichols, and Shulgin. Subsequent hearings were held with the DEA
and the Office of National Drug Control Policy.
In November 1992, Grob's revised protocol received a green light.
Then, a year later, the FDA approved a human trial with Ibogaine, a
plant-derived psychoactive compound used for treating drug addiction.
"Those early studies showed us it was possible to conduct psychedelic
research in an above-ground, sanctioned manner, and that regulators
were willing to do an objective assessment of the relative merits and
safety of studying Schedule I drugs," Grob says.
With the FDA now open for business, psychedelic researchers wasted no
time staffing up. MAPS had MDMA covered, but that still left a slew of
other psychedelic drugs that needed the imprimatur of legitimacy.
Nichols wanted to do for psilocybin what Doblin was doing for MDMA. That
meant building a new organization of his own.
Founded in 1993 and named for German chemist Arthur Heffter,
who identified mescaline as the hallucinogenic component of the peyote
cactus, the U.S.-based Heffter Research Institute is, along with MAPS,
one of a handful of major nonprofits currently leading the new wave of
psychedelic research.
Nichols is Heffter's founder and president, and he currently serves
on the faculty at the University of North Carolina at Chapel Hill. "When
we set up Heffter," he says, "we said, 'Let's not repeat the mistakes
of the 1950s and '60s. We need credentialed investigators and big-name
institutions.'"
In the early days, Nichols kept Heffter under the radar out of
concern that "some congressman would learn we wanted to treat dying
people with psychedelic hallucinogens and try to stop it." Even if drug
warriors didn't sabotage researchers directly, Nichols worried they
would put pressure on the universities where psychedelic researchers
were stationed. That backlash never occurred, but Heffter was designed
to overcome exactly those sorts of political and social barriers.
Modern psychadelic research is built almost entirely around
overcoming these obstacles. Even into the late 1990s, most psychedelic
research was happening in academic settings or even underground.
"We said, 'Let's not repeat the mistakes of the 1950s and '60s. We need credentialed investigators and big-name institutions.'"
Then in 2000, Doblin gave a presentation in California on his plan to
turn MDMA into a prescription drug. In the audience was a
pharmaceutical researcher named Amy Emerson. A geneticist by training,
Emerson had spent the past decade working on cancer drugs and vaccines
for Chiron Corporation, now a subsidiary of the pharmaceutical goliath
Novartus. But having seen firsthand "the benefits in people I care
about," she says, what she really wanted to do was work in psychedelics.
Doblin needed someone who could steer MDMA through the FDA's New Drug
Application process. Emerson knew exactly how that process worked. She
sent Doblin her resume and helped draw up some early research plans. In
2003, Doblin officially brought Emerson into the fold. Working
part-time, her goal was to do anything she could to make MAPS' work look
like conventional industry studies.
In 2009, Emerson became the executive director and director of
clinical research at the MAPS Public Benefit Corporation, a sister
organization overseeing the MDMA trial. Under her direction, MAPS has
evolved from an upstart advocacy group into a biotech startup, boasting a
digital monitoring system and multiple alumni from the pharmaceutical
industry.
"We're very similar to the biotech model," she says. "We look like every other research company."
MAPS and Heffter consider themselves friendly competitors, but they
frequently share information, including strategy, protocols, and
in-house documents. They also share the goal of building reputable
organizations that can't be tied to dangerous nightclub escapades or
hippie spiritualism.
"The paradigm for setting up Heffter was to do it in such a way that
we wouldn't be criticized when people learned what we were doing,"
Nichols says. "We'd be able to tell our critics, 'Look, we have Ph.D.s
and M.D.s. We vet all our grant proposals and we send all our studies
out for peer review.' Basically, it was the medical model."
How Psychedelic Medicine Works
The challenge for a medical model is that it requires treating
psychedelics like any other pharmaceutical product—which is to say, like
science, with clear mechanisms of action and a demonstrable chain of
cause and effect. And when it comes to psychedelic drugs, even those
synthesized in a lab and administered by researchers in white coats,
that is not always easy, in part because their use has long been linked
with mysticism, and in part because psychedelic researchers face a
scientific challenge: Although they know that the drugs do work, they
have not always understood how. Theories, however, abound.
Many of them come from Ben Sessa, a British psychiatrist and
MDMA-assisted psychotherapy researcher who also spoke at Psychedelic
Science 2017. He sees an urgent need to contextualize psychedelic
research findings within 21st century medical thinking. He is more eager
than some of his peers to break the psychedelic experience down into
its biological components.
During his lecture, Sessa displayed a chart outlining how MDMA works
as a therapeutic drug. By increasing serotonin, it catalyzes a positive
mood and creative thinking; increases in dopamine and norepinephrine,
meanwhile, stimulate patients and render them more amenable to talk
therapy; the increase in alpha-2 activity allows the patient to remain
calm and relaxed while discussing traumatic memories; the drug's
interaction with the hypothalamus, meanwhile, causes the release of
oxytocin, which leads to a sense of connection and trust with the
therapist.
In the near future, Sessa plans to take his biological research one
step further. His team plans a first-of-its kind randomly controlled and
double-blind test of the hypothesis that the psychological
transformation MDMA patients experience stems from a role reversal
between the amygdala, the part of the brain that controls fear, and the
prefrontal cortex, the part that controls higher reasoning.
Sessa's work is based on a 2012 study that found that the amygdalas
of PTSD patients essentially go into overdrive when they're reminded of
the experience that traumatized them. Meanwhile, the prefrontal cortex,
which might allow them to understand the experience as a typical memory,
is muted. Essntially, their brains are wired to cause them to
re-experience the trauma as if it is actually happening again.
Psychedelic researchers believe MDMA overcorrects this imbalance,
dramatically increasing prefrontal activity and minimizing amygdala
activity, thus allowing patients to calmly talk through their
experiences. The study is not necessary, according to Sessa, for Britain
to change its drug policies. "But it's interesting science for sure."
For other psychedelic researchers, focusing on the biological
component can feel too much like treating psychedelics as if they were
pharmaceutical products. Drug companies play a minimal role in current
psychedelic research efforts, as all the compounds mentioned in this
story are off-patent.
But if you want to talk about something other than the activation of
neurological receptors and still be taken seriously by the medical
establishment, what exactly do you talk about?
Leor Roseman, a Ph.D. candidate at Imperial College London who
studies psilocybin and neuroimaging, has also struggled with bridging
the gap between the legacy of psychedelics and modern medicine.
"When you give antidepressants," he says, "you say these are
modulating the serotonergic system, therefore people are less depressed.
With psychedelics, the explanation is that they promote, in the right
set and setting, a certain experience. That experience involves a brain
change which leads to long-term effects."
Emphasizing the biological correlate may be a sound diplomatic move,
in other words, but it comes at the cost of distinguishing what makes
psychedelic therapy so effective. But Roseman has a theory for solving
this problem.
"Ask a medical doctor, 'What is PTSD?' and the answer they'll give is
that it's a strong change in a person due to an experience. What you're
trying to do with a psychedelic is reverse that change. You use the
psychedelic to promote a certain experience, and that experience—not
just the drug, the experience—is what causes the change. If you
believe that a person can be altered by one bad experience, you should
also be willing to believe that a person can change from one beautiful,
cathartic, emotionally unitive experience."
The MDMA Experience
To those who have never undergone this sort of transformational
experience, this might sound maddeningly vague, bordering on the kind of
spiritualism psychedelic researchers say they want to avoid. Is this
really science? Is this really medicine?
I believe it is, because I have had such an experience myself.
Last year, I obtained a small amount of crystallized MDMA from a
friend of a friend. (No one associated with any of the psychedelic
researchers mentioned in this story or the broader research movement,
which discourages the kind of unsupervised experimentation I am about to
describe, was involved.) I placed it under my tongue and allowed it to
dissolve. It tasted terrible.
After 30 minutes or so, I began to feel a brewing happiness and
increasing energy. My senses heightened as I "came up." Lights became
brighter, sounds became crisper, and everything I touched—including the
skin on my face and the door handle of my apartment—felt pleasant.
Even though this was a smaller dose than is being used in clinical
trials, I now understand its value as an adjunct to psychotherapy. More
than anything, the drug made me want to talk, and to be honest with
myself and the person I was talking to. I felt both confident and calm,
and was able to rationally discuss experiences that used to fill sober
me with shame and fear. I could talk about my struggle with obesity, a
lifelong problem. I could talk about growing up in a broken home. I
could talk about the profound anxiety that has plagued me on and off
since adolescence. Those issues are not exactly solved, but I'd like to
think I have a better handle on them now than I did before my
experiment.
This is why MDMA has shown such promise as a psychotherapeutic tool.
Combined with a skilled conversation partner, I was able to examine
difficult memories without re-experiencing the volatile emotions that
made them memorable in the first place.
More than anything, the drug made me want to talk, and to be honest with myself and the person I was talking to.
Many illicit users have reported similarly positive experiences with
MDMA—or what they thought was MDMA—in the ideal "set and setting,"
Leary's shorthand for mindset and environment. Clinical trial enrollees
participating in MAPS' study for PTSD, meanwhile, reported that MDMA-assisted therapy saved their lives.
To be sure, others have reported more troubling outcomes. Writing in Rolling Stone, reporter Mac McClelland profiled the black market
for illegal psychedelic-assisted therapy, in which licensed American
medical doctors, convinced that the regulatory process is moving too
slowly, clandestinely administer MDMA within their own practices. The
experience she had with such a practitioner was not nearly as positive
as my own.
MDMA did leave me feeling mildly depressed the following morning.
That feeling is somewhat common among recreational users, and typically
lasts for one to several days after the drug's effects have worn off.
This is one reason clinical trial protocols for MDMA-assisted
psychotherapy provide patients with only two doses total. The other
reason is that, unlike with SSRIs, which depressed and anxious patients
take daily, early trials have found that MDMA requires only a couple of
doses, in conjunction with psychotherapy, to achieve positive long-term
outcomes.
Legalization and Legitimacy
For most people, those improvements can only occur if the drug is
legalized for medical use. That time, however, may be coming soon.
Starting this year, phase-three clinical trials for MDMA will begin
with a goal of ultimately enrolling somewhere between 200 and 250
patients across 14 sites in the U.S., Canada, and Israel. Emerson, the
former pharmaceutical researcher who is leading the study, is focused on
maintaining its scientific integrity. "We want to do everything up to
snuff," she says. "There can be no question about our methods." MAPS has
jumped through numerous hoops since Grob submitted his first protocol
in the early '90s, and the group has more work to do. But the end is in
sight.
In May, Doblin met with the FDA to go over MAPS' protocol for its
stage-three trial. After the meeting, Doblin emailed his staff with good
news: "Every single thing we proposed was acceptable to FDA." He signed
his email, "happily, Rick."
For Doblin, it represents a life's effort, and a conscious decision
as a young man to work within the system rather than against it. "I saw
early on the value of scientific research and fully believed in the idea
of working through the FDA's clinical research procedures to obtain
approval for prescription use," he says. "I'd seen the backlash against
the '60s and realized that incremental change, evolutionary rather than
revolutionary, was going to be required. I just didn't realize I'd still
be working towards the medicalization of psychedelics 45 years later!"
Although Leary couldn't see it in the summer of 1969, it is this
approach that has brought the psychedelic community to the brink of
legalization and legitimacy. Indeed, there is something of the
psychedelic experience embedded in the ethos of MAPS and its fellow
travelers: Their work is collaborative, transparent, self-aware, humble,
generous, and positive. It is open and accepting of the world without
trying to make it something that it is not.
"Ask your best questions," Doblin told the attendees at Psychedelic
Science 2017. "Be really responsive to the fears and anxieties of the
larger culture, and let's see how we can address them. Bring your best,
most critical, but open-minded, open-hearted selves to bear on the
conference."
"If we do that," he said, smiling like his 18-year-old self, "this can become more than a dream."
Photo Credit: Joanna Andreasson

No comments:
Post a Comment