Take a look at that image. we see an impossible straight line of visible plasma. just a month ago as well.. 3000 light years in length.
Now understand we are looking at a pulse of photonic energy leaving an event horizon at light speed and dropping decay particles along its path,. nothing happened here that is sub light except the decay radiation of the produced matter.
good history here of black hole thinking. Of course my postings point out that a black hole mostly should look like a Quasar again pumping out a full spectrum and decay possibilities we no not see.
simply put, matter arrives at an event horizon and often leaves at the speed of light as photonic energy to decay outside the original gravity well. These wells likely burn out after consuming all fuel which may well be never..
Stars behaving absurdly
For centuries, the only way in which to illuminate the mysteries of black holes was through the power of mathematics
A 3,000-light-year-long jet of plasma blasting from the M87 galaxy’s 6.5-billion-solar-mass central black hole, captured by the Hubble Space Telescope, September 2024.
is a freelance science writer living in Cambridge, Massachusetts. His articles have appeared in numerous magazines, including Quanta, Discover and Astronomy. He is the co-author, with Shing-Tung Yau, of The Gravity of Math: How Geometry Rules the Universe (2024), from which this essay was adapted.
is the director of the Yau Mathematical Sciences Center at Tsinghua University in Beijing, China and professor emeritus at Harvard University in Massachusetts, US. He is the co-author, most recently, of The Gravity of Math: How Geometry Rules the Universe (2024).
3,900 words
Email
Save
Post
Share
As celestial entities go, black holes are, paradoxically, both commonplace and extraordinary. They could be seen as commonplace due to their general ubiquity. Astrophysicists now believe that giant black holes – each with the mass of millions or billions of suns – inhabit the centres of practically every large galaxy, where they exert a powerful influence over star formation and other processes. There are more than 200 billion such galaxies, according to estimates, each thought to harbour about 100 million stellar- or star-sized black holes. Adding that up, we’re talking about something on the order of 1019 – or 10 billion billion – black holes. And far into the future, when the Universe is three times its current age (or about 40 billion years old), black holes will be all that’s left. That prediction was made in an analysis by the astrophysicists Fred C Adams and Gregory Laughlin in 1997 who concluded that, in the distant future, ‘the only stellarlike objects remaining [will be] black holes of widely disparate masses.’

The Event Horizon Telescope provided the first direct visual evidence of the supermassive black hole in the centre of Messier 87 and its shadow. Courtesy Wikipedia
On the other hand, black holes are also extraordinary. They’re the densest known objects in the Universe. The Sun, for instance, would be a black hole if all its matter were squeezed into a radius of less than 3 kilometres, rather than its actual radius of about 700,000 kilometres – a hypothetical compacting that would make our host star more than 10 quadrillion times denser than it is right now. Because matter in a black hole is, by definition, compressed into a relatively tiny space, its gravitational field is so strong that not even light can escape its indomitable grip. And that is why such an object is called ‘black’. Light cannot get out from the interior of a black hole, which means there is no possible way to look inside.
In view of the ineluctable opacity of black holes, one might wonder how we’ve managed to learn anything about them – especially when it comes to insights regarding their interior structure. While it’s certainly true that vital clues have been obtained from observational data, empirically obtained information has become available only in recent decades. However, for a period of about 200 years prior to that, all we had to rely on were physical theories and mathematics, and that’s the story we are telling here. From the late 18th century to the present day, mathematicians have tackled questions about these enigmatic objects that are beyond the range of any telescope yet devised – questions limited only by the reach of human imagination.
Join over 250,000+ newsletter subscribers
Our content is 100 per cent free and you can unsubscribe anytime.
Daily: A daily dose of essays, guides and videos from Aeon+Psyche
Weekly: A week’s worth of big ideas from Aeon
Sign up
The very concept of black holes was invented through mathematics by the visionary, if little-known, scientist John Michell in 1783 (though he did not call them black holes at the time). In 1750, this low-profile rector of a small English village (Thornhill, 20 miles south of Leeds) demonstrated that the force between two magnetised objects drops off with the square of the distance between them – which was about three decades before the French scientist Charles-Augustin de Coulomb established that same fact. And in 1755, Michell proposed that earthquakes generate waves that propagate through the earth, ‘thereby helping establish the field of seismology’, according to the American Physical Society. Michell was the first to use statistical methods to demonstrate that stars often group together in binary pairs or in larger assemblages. He also conceived of a device for measuring the strength of gravity between two objects, which was used in a renowned experiment by Henry Cavendish in 1798, five years after Michell’s death.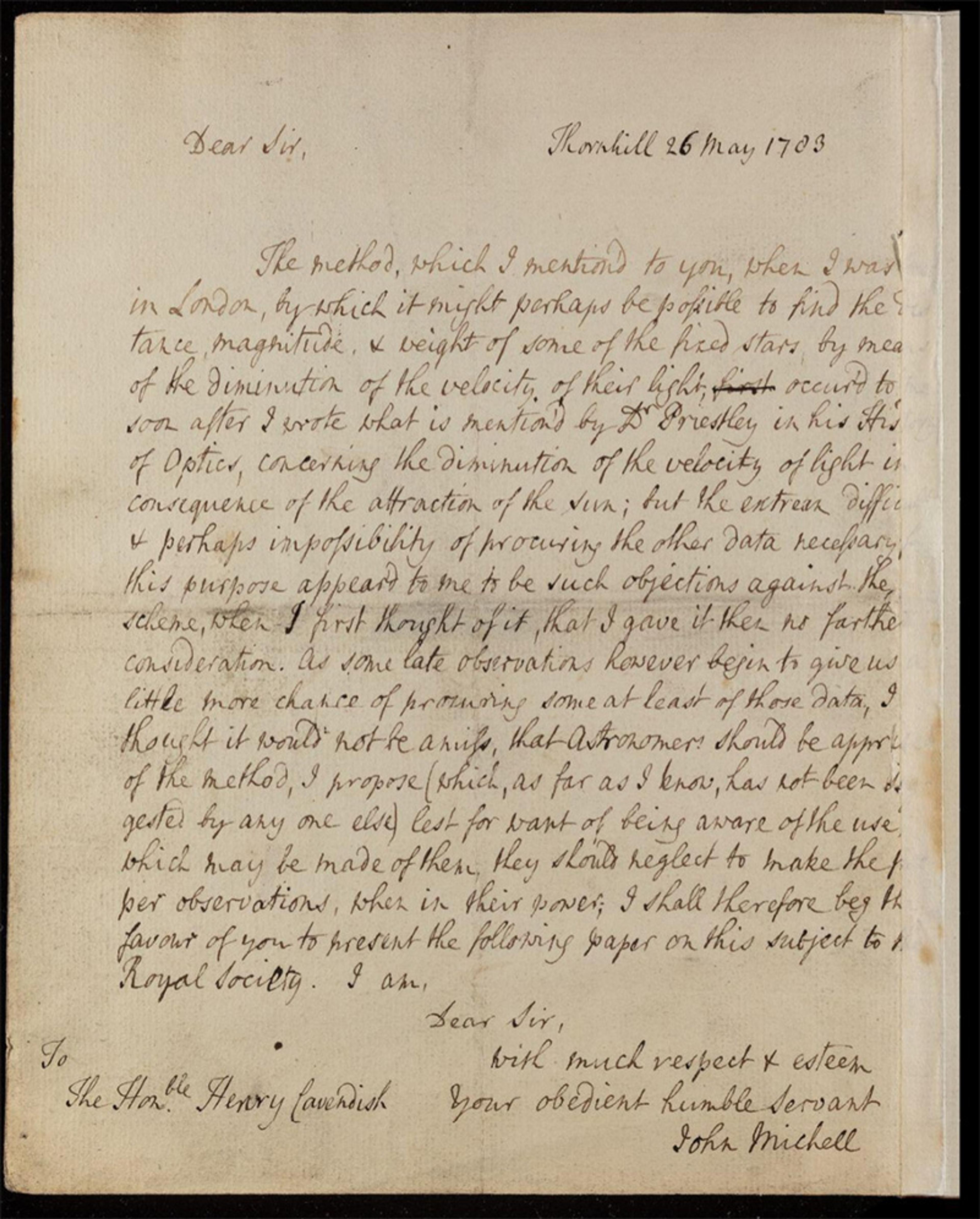
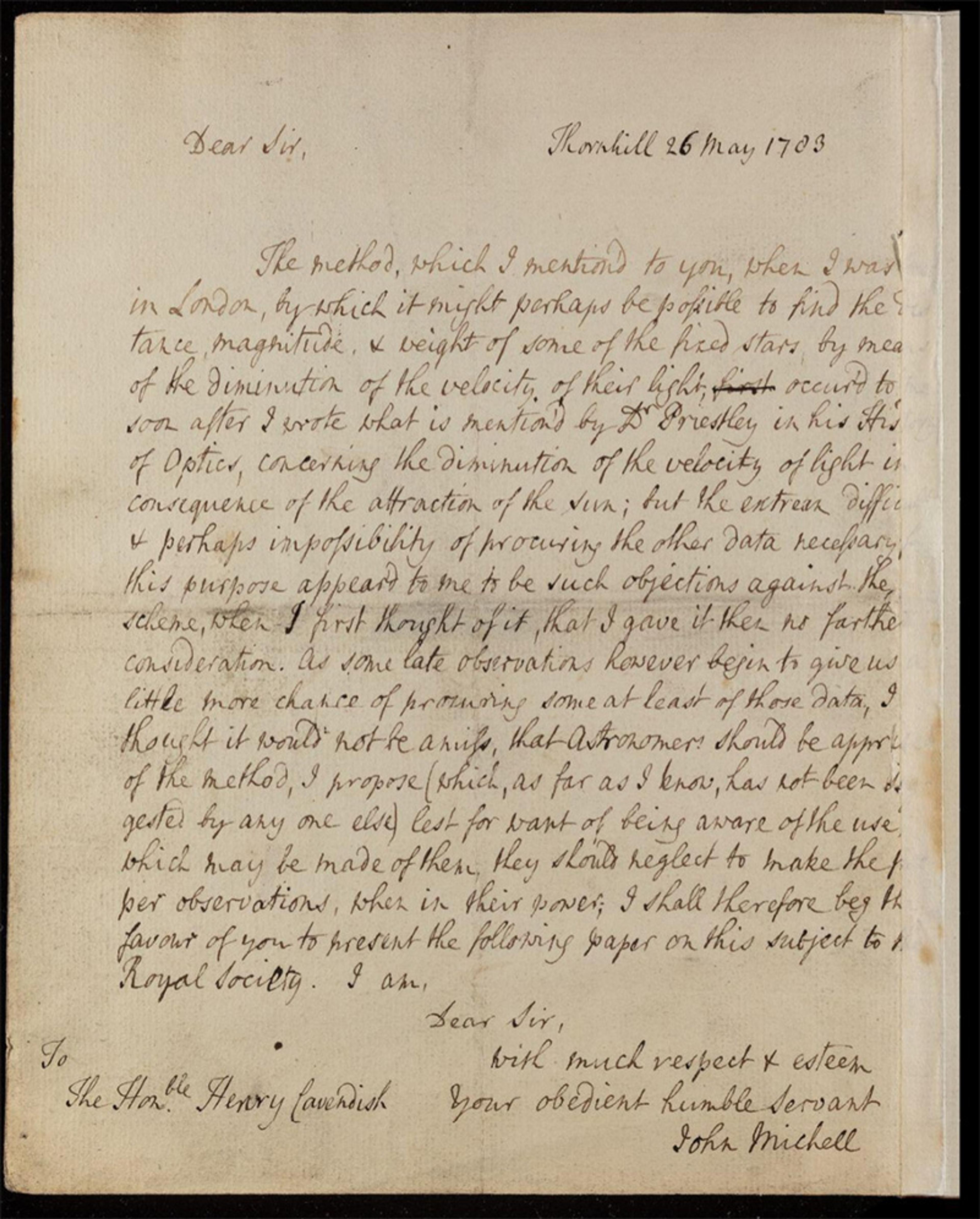
Mitchell’s November 1783 letter to Cavendish and published in Philosophical Transactions, as ‘On the means of discovering the distance, magnitude, &c. of the fixed stars, in consequence of the diminution of the velocity of their light, in case such a diminution should be found to take place in any of them, and such other data should be procured from observations, as would be farther necessary for that purpose.’ By the Rev. John Michell, B.D. F.R.S. Courtesy the Royal Society, London
Michell was ahead of his time on all these fronts, but the ideas he conveyed in a 1783 letter to Cavendish – published a year later in the journal Philosophical Transactions – were more than a century ahead of the curve. Michell was originally motivated to devise a technique for determining the mass of a star. He subscribed to a theory, first advanced by Isaac Newton, that light consisted of a stream of particles known as corpuscles. He surmised that the gravitational pull of a star would slow the motion of these light particles. And if the star was big enough – ‘more than 500 times the diameter of the Sun’, he calculated – ‘all light emitted from such a body would be made to return towards it, by its own proper gravity.’ The gravitational field in such a case would be so strong that it would overcome the escape velocity of light itself, Michell proposed.
Their escape velocities are, indeed, greater than the speed of light
Any light produced by a star would be trapped inside, making the star invisible, but there still might be a way to detect its presence, he suggested: ‘If any other luminous bodies should happen to revolve about them, we might still perhaps from the motions of these revolving bodies infer the existence of the central ones with some degree of probability.’
In his remarkably discerning presentation, Michell got many things right about what we now call black holes. Their escape velocities are, indeed, greater than the speed of light, and the presence of many black holes has been deduced by scrutinising the motions of the luminous bodies that fall under their gravitational spell.
Through no fault of his own, however, Michell got many of the particulars wrong. We now know that the crucial determinant as to whether a star is destined to become a black hole depends on its density, not its diameter. Moreover, it was not until 1905 that Albert Einstein postulated the notion – supported by experiments both before and since – that light travels at a constant velocity and cannot be slowed down by the influence of gravity (as Michell and other 18th-century scholars had supposed). Optical experiments carried out by Thomas Young in 1801 bolstered the proposition that light had wave-like properties – evidence that led to the eventual downfall of Newton’s corpuscular theory of light.
Few scientists of Michell’s era were able to comprehend his arguments about dark, invisible stars, and his ideas consequently attracted little notice. To gain a detailed understanding of the curious objects that Michell conjured up, an entirely new way of thinking about matter, gravity, light and energy was required. That is just what Einstein provided on 25 November 1915 when he supplanted Newton’s then 230-year-old law of universal gravitation with the introduction of his own brainchild – the general theory of relativity.
Einstein offered a novel description of gravity that was, at its heart, geometrical. Gravity, he said, was not an attractive force exerted between two or more massive objects, as Newton had maintained centuries earlier. Instead, the phenomenon arose from the fact that a massive object curves the space and time around it. In this theory, space and time meld together to form the concept of ‘spacetime’ – and the curvature of spacetime, in turn, relates directly to its shape or geometry. According to Einstein’s view, it is the curvature of spacetime induced by a massive object like the Sun that holds other objects – such as the planets in the solar system – in its gravitational sway. This notion was summed up decades later by the physicist John Wheeler in his oft-cited statement: curved spacetime tells matter how to move; matter tells spacetime how to curve.
It took Einstein 10 long years to arrive at this result – during which, by his own admission, he worked harder than ever before in his life. And the outcome of this pursuit – which characterised gravity as a geometric effect – was somewhat ironic, given that Einstein had previously not held mathematics in high regard, nor had he devoted much effort to that subject area as a student. He knew little about geometry when he set out to formulate his general theory, and he had not even heard about the geometry of curved spaces invented in 1854 by the mathematician Bernhard Riemann, upon which his theory ultimately was based.
Einstein’s contribution here can be encapsulated within a single mathematical equation that might appear to be quite simple: Gij = Tij. The curvature of spacetime on the left side of this expression is equal to the distribution of matter and energy on the right. However, the letters G and T represent complex mathematical constructs known as tensors, which are 4-by-4 arrays of numbers and functions. What looks like a single equation above is, in fact, 10 linked ‘field’ equations. Each one of these equations would be difficult to solve on its own and, to make things harder, all 10 of them have to be solved simultaneously.
As the radius goes to zero, the pressure and density would approach infinity
Einstein did not know whether an exact solution to his field equations could ever be obtained. And when he used his equations to address a longstanding problem regarding Mercury’s anomalous orbit around the Sun, he sought and eventually found only approximate solutions.
Fortunately, Einstein’s paper of 25 November 1915 made its way into the hands of the physicist Karl Schwarzschild, who was then a 42-year-old soldier in the German army, assigned to the Russian front during the First Word War. Schwarzschild somehow found time during breaks in the military action not only to read Einstein’s paper but also to pursue his own ideas, which culminated in the first exact solution to the field equations of general relativity. The solution in question – which Schwarzschild sent to Einstein in a letter dated 22 December and published a month later – described the geometry of spacetime around a spherical, non-rotating star. Based on his determination of the geometry, Schwarzschild was able to work out the precise mechanics of Mercury’s orbit around the Sun, providing a mathematical description that had proven elusive until that time.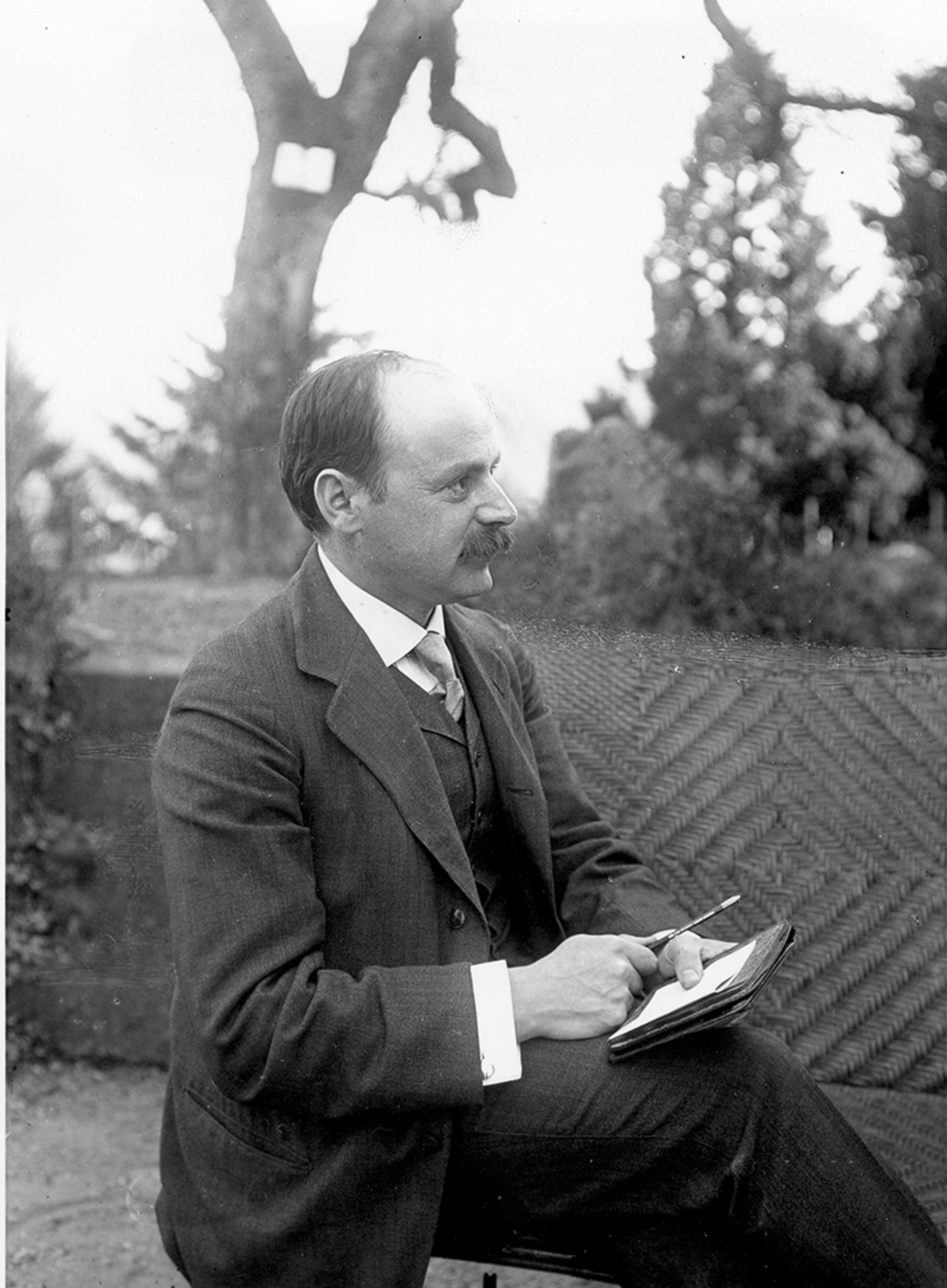
In February, Schwarzschild published a second paper in which he explored, again mathematically, the interior of such a star. Using an argument reminiscent of the approach Michell had pursued some 130 years earlier – though propped up this time by the framework of Einstein’s new gravitational theory – Schwarzschild showed that, if enough mass were packed into a small enough radius, any light produced by the star would be stuck inside. This radius, known as the Schwarzschild radius, marks the boundary of what we now call the event horizon – the point of no return, or actually the surface of no return surrounding a black hole, beyond which any light or particles cannot get out.
Of perhaps even greater interest was what Schwarzschild found at the centre of his hypothetical sphere-like star. As the radius goes to zero, the pressure and density would approach infinity. Such a point would be called a singularity – a place where the laws of general relativity would break down and its predictions would go haywire. Schwarzschild, in other words, had identified some of a black hole’s key features back when the theory of general relativity was just a few months old.
Einstein, the author of that theory, doubted that the objects that sprung from Schwarzschild’s equations could actually exist. ‘If this result were real, it would be a true disaster,’ Einstein commented, reflecting his sense that the appearance of singularities would have a pathological effect on his newly unveiled theory.
Schwarzschild considered his solution an important theoretical contribution, but he too was unsure of the physical reality of the objects that his calculations gave rise to – objects that would be called black holes 50 years later. One of his qualms was that he couldn’t think of a viable mechanism for how such things could be formed, nor did he believe that the predicted infinite pressures could ever be realised. Schwarzschild, sadly, was unable to carry this work further, as he died a few months later, in May 1916, from a disease he contracted during the war.
Although mathematical analyses, drawing on Einstein’s theory, had raised the possibility of black holes, the concept remained an abstraction until persuasive arguments could be made as to how objects of this sort might actually materialise in the real world.
Some of the earliest inklings that black holes might be real came in 1930 when a 19-year-old Indian student, Subrahmanyan Chandrasekhar, travelled by ship from Madras to Southampton. Chandrasekhar was headed for the University of Cambridge, where he would pursue graduate studies in astrophysics. It was a long journey to England and, to pass the time, his thoughts turned – as many a young man’s mind might – to white dwarfs, a kind of star he’d become interested in after reading a book on the subject by Arthur Eddington, who was then a professor at Cambridge, as well as one of the world’s most esteemed astronomers. A white dwarf is the dense core of a star (roughly the size of the Sun) that is no longer ‘shining’, having exhausted its nuclear fuel and expelled almost all of its outer layer. Chandrasekhar wanted to know how big (or massive) a white dwarf could be without collapsing uncontrollably to a singularity of infinite density. He determined during this voyage that such a gravitational instability would occur in a white dwarf of 1.44 solar masses – a threshold that’s now called the Chandrasekhar limit.
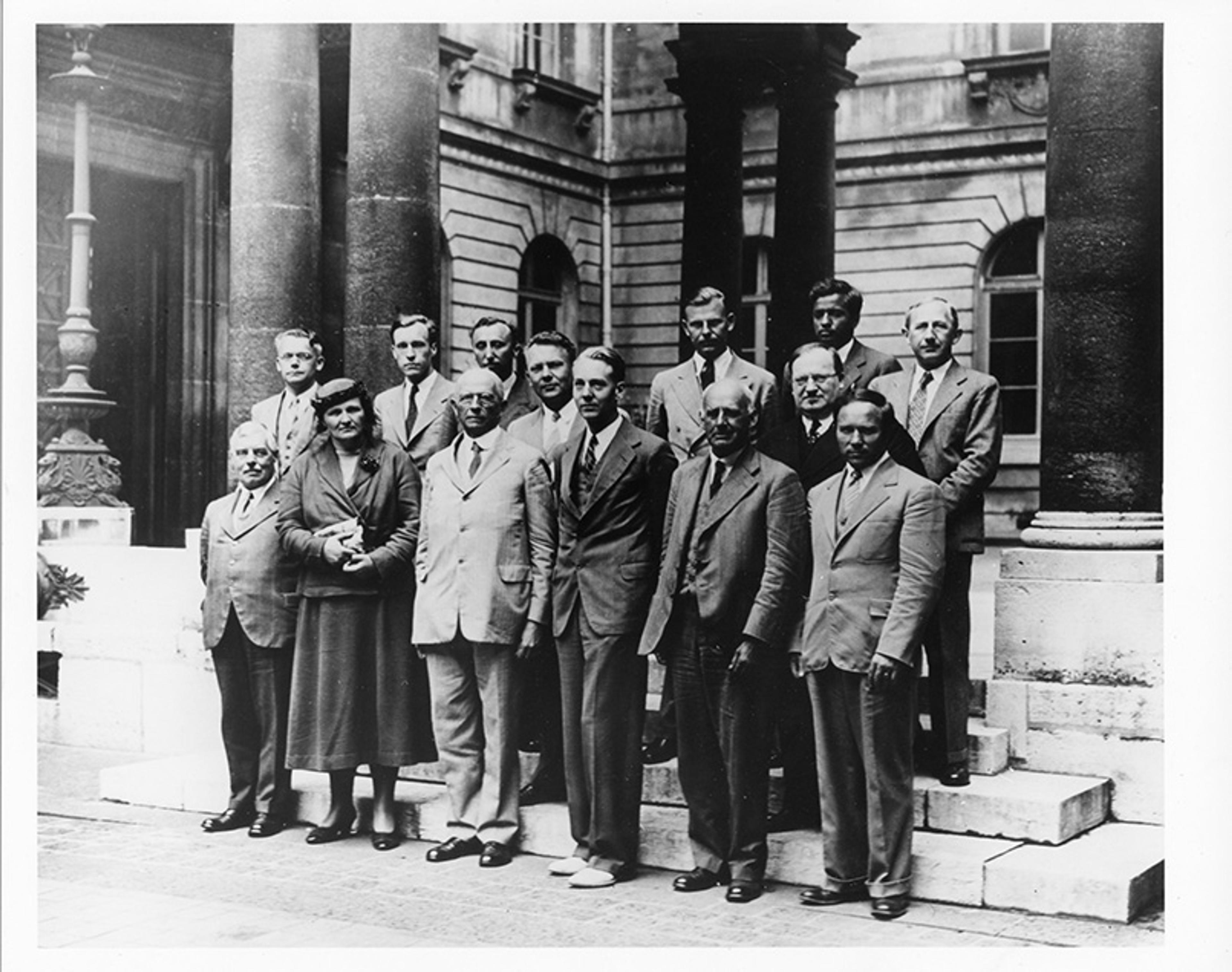
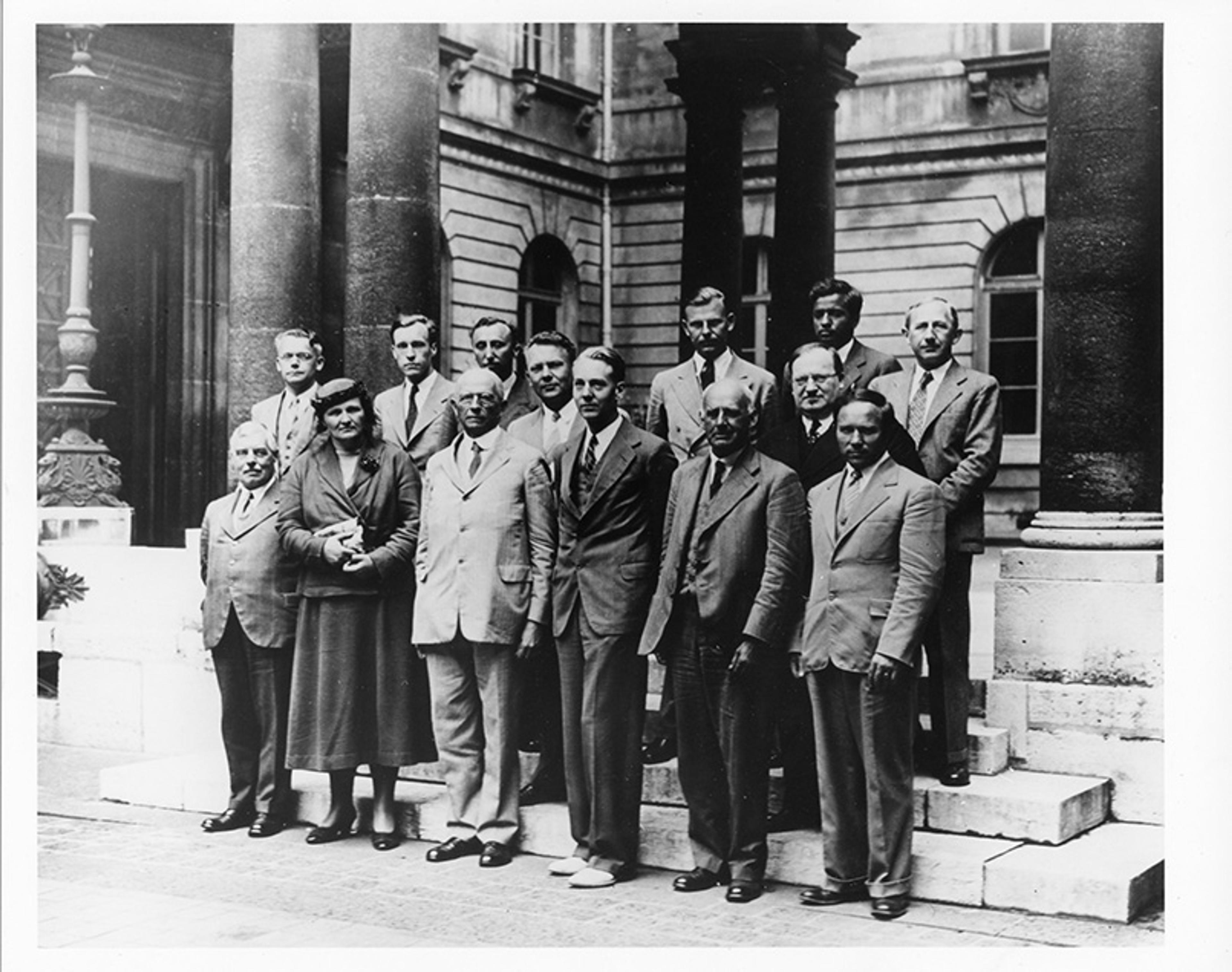
Attendees of the Astrophysical Conference on Novae and White Dwarfs in Paris, 1939. Subrahmanyan Chandrasekhar is back row, second from right, Arthur Eddington front row, second from right. Courtesy the AIP Emilio Segrè Visual Archives
He presented this result at a meeting of the Royal Astronomical Society of London, but his findings were challenged by Eddington, who declared that Chandrasekhar’s ideas – based, as they were, solely on mathematics – bore no relation to the physical world. There ought to be a law of nature, Eddington said, ‘to prevent a star from behaving in this absurd way’. Any claims to the contrary, he added, were tantamount to ‘stellar buffoonery’.
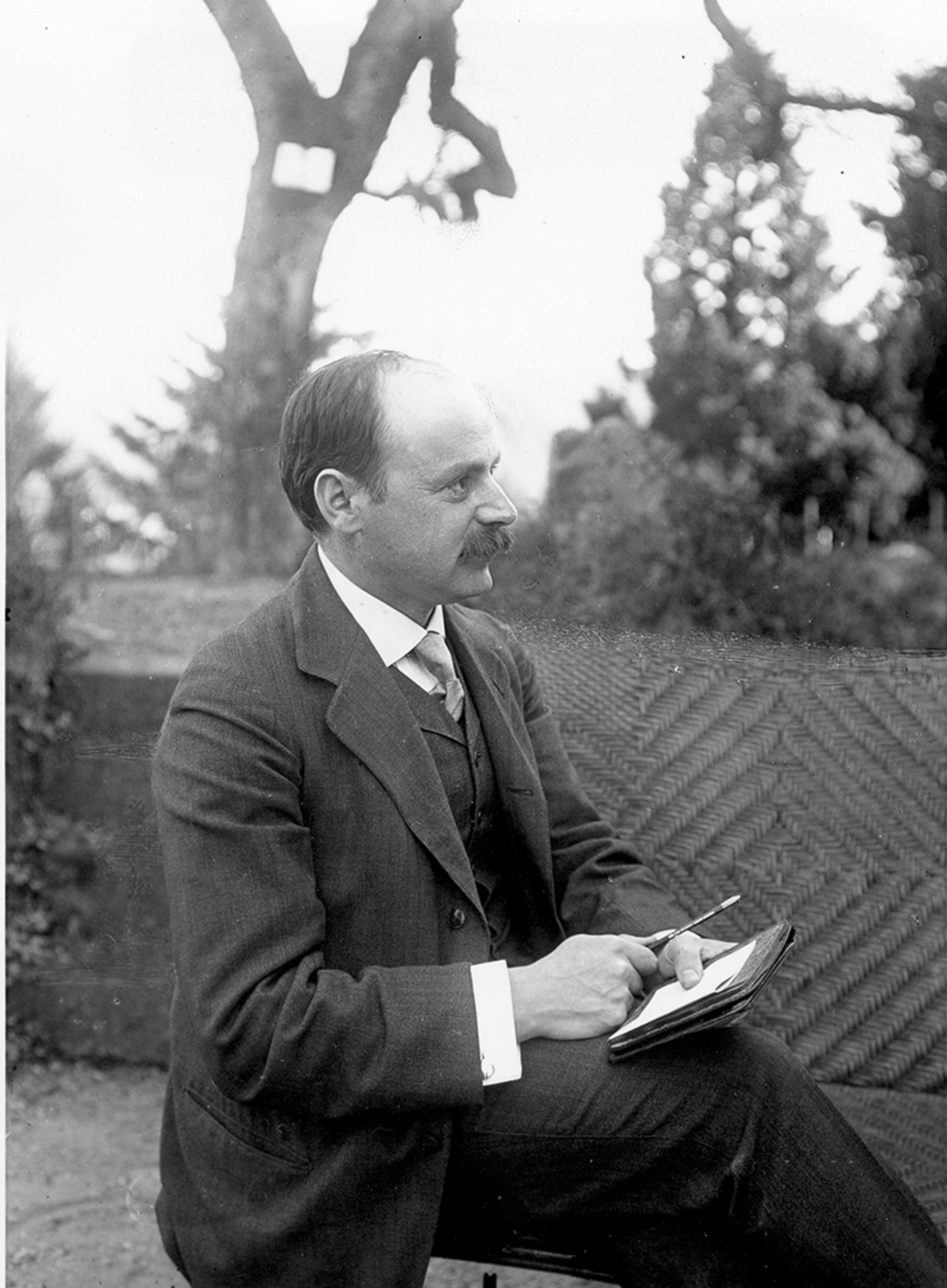
Subrahmanyan Chandrasekhar and his wife Lalitha at the McDonald Observatory in 1939. Courtesy of Special Collections Research Center, University of Chicago Library
Chandrasekhar was ultimately vindicated. He won the 1983 Nobel Prize in Physics for this and related work on stellar evolution – the same year that he published a 672-page book, The Mathematical Theory of Black Holes. History, meanwhile, has proven Eddington wrong on this point: it turns out that our laws of nature do permit stars to behave in ‘such an absurd way’. And much of that was demonstrated by the physicist J Robert Oppenheimer and his colleagues in the late 1930s.
Oppenheimer generalised Chandrasekhar’s results on mass limits to stars other than white dwarfs – specifically to neutron stars, the cores of collapsed stars that are so dense, their electrons and protons get crushed together to form neutrons. (A tiny chunk of a neutron star, the size of a sugar cube, would weigh a billion tons.) Working with George Volkoff, Oppenheimer showed that a neutron star of more than about three solar masses will inexorably collapse into a black hole.
Einstein’s arguments were eventually refuted, and he never wrote another paper on black holes
And he went further still. In a separate paper in September 1939 with his then-graduate student Hartland Snyder, Oppenheimer filled in a key part of the picture that Chandrasekhar had not addressed, supplying a step-by-step mathematical account of the process whereby a star implodes to form a black hole. The mathematician Demetrios Christodoulou regarded this achievement as ‘very significant, being the first work on relativistic gravitational collapse’. By showing how a black hole can be formed, guided by Einstein’s equations, Oppenheimer and Snyder brought the product of Schwarzschild’s wartime musings much closer to plausibility.
Ironically, one month later, in October 1939, Einstein published a paper in The Annals of Mathematics in which he claimed to have set forth ‘a clear understanding as to why the “Schwarzschild singularities” do not exist in physical reality’ – essentially challenging a prediction that was borne of his own equations. Einstein’s arguments were eventually refuted, and he never wrote another paper on black holes.
Oppenheimer did not undertake any additional work on the subject either – despite the important contributions he’d already made. By 1942, he had other weighty matters on his mind, as he was asked to join the Manhattan Project that year. In 1943, he was named director of the Los Alamos Laboratory where the atomic bomb was being developed, and that work – for obvious reasons – overshadowed his prior theorising about black holes.
Another momentous breakthrough on the mathematics front came in 1963 when Roy Kerr, a New Zealander then based at the University of Texas, addressed a major shortcoming of the Schwarzschild solution: it applied only to spherical black holes that are stationary – a problem, given that every star and planet ever observed rotates to some extent. And rotating objects are not perfectly round; they have bulges at the centre. Kerr’s colleague at Texas, Alan Thompson, warned Kerr not to waste his time and effort on spinning black holes, because a new paper by the physicist Ezra Newman and two co-authors had just concluded that no solutions could be found for them.
Upon identifying a flaw in the paper by Newman et al, Kerr forged ahead. However, in order to make progress, he had to adopt two simplifying assumptions: first, that the black holes are rotating at a constant rate so that nothing in this scenario changes in time and, second, that even though the black holes were not perfect spheres, they were still symmetrical around a vertical axis – in the same way that an upright cylinder is nonspherical yet symmetrical around its vertical axis. With these assumptions, he soon hit upon a solution to the Einstein equations that applied to rotating black holes – or Kerr black holes, as they were soon called.
Kerr’s paper, which was published in July 1963, was just a page-and-a-half long, but it was considered a huge advance because he had furnished the best mathematical representation yet of a physically realistic black hole.
Chandrasekhar praised the accomplishment, saying that Kerr’s description applied flawlessly to ‘untold numbers of massive black holes that populate the Universe’.
In the fall of 1963, the mathematical physicist Roger Penrose came as a visiting professor to the University of Texas, where he engaged in many conversations with Kerr. One thing Penrose wondered about was whether the singularities that arose in Schwarzschild and Kerr black holes would also arise in objects that lacked those same symmetries. His answer came in his 1965 singularity theorem – and in other theorems that followed (some carried out with Stephen Hawking) – which earned Penrose a Nobel Prize in Physics in 2020. To explore this question, he developed new mathematical tools from geometry and the related subject of topology (the study and classification of the general, as opposed to exact, shape of objects). In 1965, Penrose proved that the event horizon of a Schwarzschild and Kerr black hole is something called a closed trapped surface – a surface whose curvature is so intense that even outward-pointing light beams get wrapped around and forced inward. Once a closed trapped surface is formed, he demonstrated, the collapse to a singularity is inevitable, regardless of symmetry considerations.
When Penrose gave a talk at Princeton about his theorem shortly after his January 1965 paper came out, the physicist Robert Dicke told him he’d ‘shown [that] general relativity is wrong’. There was no problem with the theory, Penrose countered, ‘[b]ut you do have to have singularities’ – which was a point that many physicists, including Einstein, had been hesitant to accept.
A complementary piece of this puzzle came in a 1979 theorem (published in 1983) by the mathematicians Richard Schoen and Shing-Tung Yau. Although Penrose had proved that a closed trapped surface will evolve (or devolve) to an object with a central singularity, he did not say how a closed trapped surface could be created in the first place. Schoen and Yau spelled out the precise conditions: when the matter density of a given region is twice that of a neutron star, a trapped surface will form, and that object will collapse directly to a black hole.
Their work, now referred to as the black hole existence proof, came out at a time when the existence of black holes was still open to debate. But by then, the evidence was starting to build. In the 1970s, astronomers proposed that a bright X-ray source called Cygnus X-1 was a stellar-sized black hole, and that the galaxy M87 harboured a supermassive black hole with the mass of billions of suns. And by the 1990s, a case was starting to be made that a supermassive black hole resided at the centre of practically every large galaxy.
Mathematicians still have a big role to play in unravelling the elusive properties of black holes
The case for the physical reality of black holes was dramatically strengthened on 14 September 2015, when detectors from the LIGO Observatory in Louisiana and Washington state intercepted gravitational waves for the first time in history – the product, scientists asserted, of the violent collision of two black holes, each with the mass of about 30 suns, which took place about 1.3 billion light-years from Earth (and hence about 1.3 billion years ago). Gravitational waves from roughly 100 other collisions and mergers – involving black holes and their ultra-dense kin, neutron stars – have since been detected.
In 2019, a global network of radio telescopes that collectively comprise the Event Horizon Telescope captured an image of the outer edge of an enormous black hole (with the mass of billions of suns) lying in the centre of the M87 galaxy. In 2022, the Event Horizon Telescope obtained an image of the ‘supermassive’ black hole in the centre of our own galaxy, the Milky Way, with the mass of 4 million suns.
In view of this and other compelling evidence, the existence of black holes is no longer a matter of dispute among astrophysicists. But that should not be taken to mean that our understanding of these objects is complete. Nothing could be further from the truth. And mathematicians still have a big role to play in unravelling the elusive properties of black holes.
To cite a recent example, in 2022, the mathematicians Elena Giorgi, Sergiu Klainerman, and Jérémie Szeftel proved that slowly rotating Kerr black holes are stable, meaning that if you perturb a Kerr black hole in a gentle way, by giving it a little ‘bump’, it will settle down and behave in just the way the Kerr solution prescribed. In 2023, Marcus Khuri and Jordan Rainone proved that an infinite family of black holes, configured in a variety of elaborate shapes, are mathematically possible in higher-dimensional spaces that extend beyond the three familiar dimensions. While such exotic entities are by no means certain to exist, there is nothing in mathematics that rules them out.
Meanwhile, there are several open problems concerning black holes that have kept mathematicians busy for more than half a century. One is the cosmic censorship conjecture, first posed by Penrose in 1969, which holds (in one of its various forms) that singularities must be concealed behind an event horizon. Or, to put it more starkly, there are no ‘naked’ singularities. The second problem relates to the no-hair theorem (or actually conjecture), which posits that black holes can be fully characterised by their mass, spin and charge. Restating that in slightly different terms, there is no way to distinguish between two black holes that have the same mass, spin and charge. Special cases have been solved for both of these enduring problems, but there are no complete solutions for either of them.
Scientists still have deeply profound questions about black holes. And though technology has finally enabled us to glimpse the tumultuous exteriors of these objects, mathematics is often all we have to illuminate those places that our instruments cannot penetrate – including the shadowy realm, deep inside a black hole, that is otherwise obscured by an event horizon.