
It make perfect engineering sense and it explains our remarkable ability to recover from insult and because draining fluids collapses this network, it has not been identified at all until now.
The Interstitium, the Largest Organ We Never Knew We Had
The human body was thought to have 79 organs—until researchers stumbled on a strange phenomenon that could turn medicine and what we thought we knew about the body upside down.
TANYA BASU
03.27.18 5:11 AM ET
https://www.thedailybeast.com/meet-the-interstitium-the-largest-organ-we-never-knew-we-had
A study published in Scientific Reports on Tuesday suggests that a previously unknown organ has been found in the human body.
More astonishingly, the paper puts forth the idea that this new organ is the largest by volume among all 80 organs—if what the researchers found is, in fact, an organ.
How could what’s being termed as the largest organ in our body escape notice for so long? A dogged trio of researchers stumbled upon it—despite the fact that they argue it’s a crucial part of our bodies and been there all along, right in front of us. It’s an astounding find—but not without controversy.
When I first met Neil Theise at a busy, east side Manhattan deli in the middle of the work day last November, I was embarrassingly late, having budgeted 15 minutes for what turned out to be an hour-long trip. Theise—unassuming in a scrunched shirt and jacket—cheerfully waited, but I was late enough that he’d started eating a hot, open-faced turkey sandwich with gravy, while jovially chatting with the wait staff (“I’ve been coming here since I was a kid!” he announced).
Between slurps of soup, Theise told me that he’d been working on several medical studies for the past few years. He was a Jewish Buddhist, a man who was at home with discussing the various veins of meditative practices in the same breath as the intricacies of liver pathology.
Out of nowhere, he told me that he’d stumbled upon a hidden organ.
A study published in Scientific Reports on Tuesday suggests that a previously unknown organ has been found in the human body.
More astonishingly, the paper puts forth the idea that this new organ is the largest by volume among all 80 organs—if what the researchers found is, in fact, an organ.
How could what’s being termed as the largest organ in our body escape notice for so long? A dogged trio of researchers stumbled upon it—despite the fact that they argue it’s a crucial part of our bodies and been there all along, right in front of us. It’s an astounding find—but not without controversy.
When I first met Neil Theise at a busy, east side Manhattan deli in the middle of the work day last November, I was embarrassingly late, having budgeted 15 minutes for what turned out to be an hour-long trip. Theise—unassuming in a scrunched shirt and jacket—cheerfully waited, but I was late enough that he’d started eating a hot, open-faced turkey sandwich with gravy, while jovially chatting with the wait staff (“I’ve been coming here since I was a kid!” he announced).
Between slurps of soup, Theise told me that he’d been working on several medical studies for the past few years. He was a Jewish Buddhist, a man who was at home with discussing the various veins of meditative practices in the same breath as the intricacies of liver pathology.
Out of nowhere, he told me that he’d stumbled upon a hidden organ.
“An organ?” I asked, incredulous. “But haven’t we discovered them all?” In January 2017, researchers at the University of Limerick published their defining of a fold in the lining of the abdomen as a new organ in The Lancet.
But this wasn’t the same. Theise smiled, expecting the reaction, and knowing that I probably thought he was making something up or more likely had severely exaggerated something much more tame and inane. Theise said that he’d not only found a new organ, he’d found what he estimated to be the largest organ by volume, only increasing my confusion—and skepticism.
The new organ, he explained, was a thin layer of dense connective tissue throughout the body, sandwiched just under our skin and within the middle layer of every visceral organ. The organ also made up all the fascia, or the thin mesh of tissue separating every muscle and all the tissue around every vein and artery, from largest to smallest. What initially seemed to be a solid, dense, connective tissue layer was actually a complex network of fluid-filled cavities that are strong and flexible, yet so tiny and undiscerning that they escaped the attention of the brightest scientific minds for generations.
In fact, Theise expanded, this “interstitium” could explain many of modern medicine’s mysteries, often dismissed by the establishment as either silly or explainable by other phenomena. Take acupuncture, Theise said—that energetic healing jolt may be traced to the interstitium.
Or perhaps the interstitium acted as a “shock absorber,” something that protected other organs and muscles in daily function. Also, the space is in direct communication with the lymphatic system as the origin of lymph fluid—which means the interstitium’s system of fluid-filled backroads could explain the metastasis of cancer cells and their quick spread beyond the limits of the organ in which the cancer started.
The man scarfing down a turkey sandwich before me in a New York deli claimed to not only have stumbled upon an organ, but the largest one in our body, something that was sure to change not just medical textbooks but the way we understood everything from cancer to acupuncture to inflammation. It was astonishing, almost too good to be true. Was it real?
One day nearly four years ago, David Carr-Locke and Petros Benias, endoscopists— specialists that insert an endoscope directly into an organ to examine it—approached Theise. Theise was a liver pathologist at Mount Sinai Beth Israel Hospital’s Digestive Disease Division at the time, and they were nerding out together; Theise called Carr-Locke a “technology junkie,” someone who was obsessed with checking out the latest medical equipment.
That the three had a close friendship as well as professional relationship is not surprising; their work, after all, was intertwined. Endoscopists like Carr-Locke and Benias collect samples from organs and pathologists like Theise analyze them. Endoscopists tend to look at surface-level tissue, while pathologists look deeper, at the entirety of an organ.
That fateful day, Carr-Locke and Benias approached Theise with an unusual image, one that had been puzzling them. A new endoscope they were using allowed microscopic viewing of living tissues, not just the dead tissues removed at surgery or biopsy and transformed into a microscope slide. Carr-Locke and Benias gathered the sample from living tissue just before taking a biopsy. They used a green dye called fluorescein, which spreads through the body when infused into a vein and allows an endoscopist to clearly see differences in microscopic, closely set structures to a depth of less than a tenth of a millimeter, or the thickness of seven sheets of paper.
But this wasn’t the same. Theise smiled, expecting the reaction, and knowing that I probably thought he was making something up or more likely had severely exaggerated something much more tame and inane. Theise said that he’d not only found a new organ, he’d found what he estimated to be the largest organ by volume, only increasing my confusion—and skepticism.
The new organ, he explained, was a thin layer of dense connective tissue throughout the body, sandwiched just under our skin and within the middle layer of every visceral organ. The organ also made up all the fascia, or the thin mesh of tissue separating every muscle and all the tissue around every vein and artery, from largest to smallest. What initially seemed to be a solid, dense, connective tissue layer was actually a complex network of fluid-filled cavities that are strong and flexible, yet so tiny and undiscerning that they escaped the attention of the brightest scientific minds for generations.
In fact, Theise expanded, this “interstitium” could explain many of modern medicine’s mysteries, often dismissed by the establishment as either silly or explainable by other phenomena. Take acupuncture, Theise said—that energetic healing jolt may be traced to the interstitium.
Or perhaps the interstitium acted as a “shock absorber,” something that protected other organs and muscles in daily function. Also, the space is in direct communication with the lymphatic system as the origin of lymph fluid—which means the interstitium’s system of fluid-filled backroads could explain the metastasis of cancer cells and their quick spread beyond the limits of the organ in which the cancer started.
The man scarfing down a turkey sandwich before me in a New York deli claimed to not only have stumbled upon an organ, but the largest one in our body, something that was sure to change not just medical textbooks but the way we understood everything from cancer to acupuncture to inflammation. It was astonishing, almost too good to be true. Was it real?
One day nearly four years ago, David Carr-Locke and Petros Benias, endoscopists— specialists that insert an endoscope directly into an organ to examine it—approached Theise. Theise was a liver pathologist at Mount Sinai Beth Israel Hospital’s Digestive Disease Division at the time, and they were nerding out together; Theise called Carr-Locke a “technology junkie,” someone who was obsessed with checking out the latest medical equipment.
That the three had a close friendship as well as professional relationship is not surprising; their work, after all, was intertwined. Endoscopists like Carr-Locke and Benias collect samples from organs and pathologists like Theise analyze them. Endoscopists tend to look at surface-level tissue, while pathologists look deeper, at the entirety of an organ.
That fateful day, Carr-Locke and Benias approached Theise with an unusual image, one that had been puzzling them. A new endoscope they were using allowed microscopic viewing of living tissues, not just the dead tissues removed at surgery or biopsy and transformed into a microscope slide. Carr-Locke and Benias gathered the sample from living tissue just before taking a biopsy. They used a green dye called fluorescein, which spreads through the body when infused into a vein and allows an endoscopist to clearly see differences in microscopic, closely set structures to a depth of less than a tenth of a millimeter, or the thickness of seven sheets of paper.
Carr-Locke
and Benias were viewing the large duct that drains bile from the liver
to the gut and saw what seemed to be a “reticular pattern”: dark bands
that separate what Theise called “oddly shaped bright spaces.”
“What is that?” they asked Theise.
At
first, the three of them agreed what they were looking at looked like
capillaries. “But if they were capillaries, the capillary structures
would be bright—filled with the fluorescent dye—and the spaces between
them would be dark,” Theise realized. “This was the reverse.”
Endoscopists
who had been reporting this pattern had made guesses in their published
papers about what they were, none of which made sense to the group.
Theise reached out to his histology books from medical school. “None of
them had pictures of the bile duct outside of the liver, because,
really, who cares about the anatomy of a bile duct?” he said.
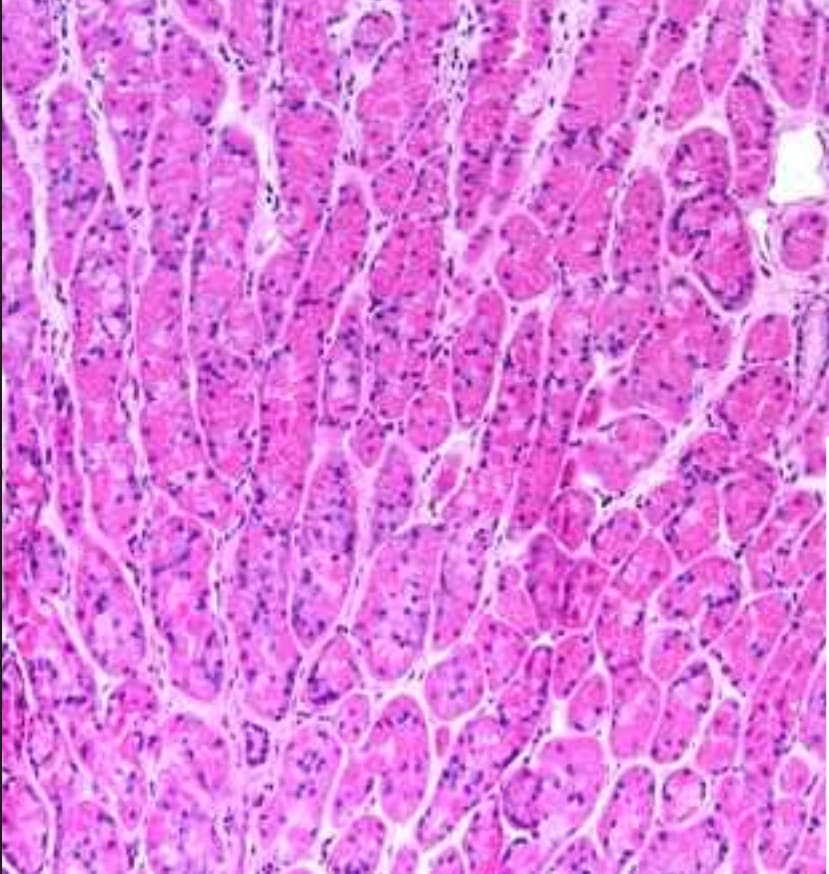
They
went back to the basics, referring to old medical textbooks. They pored
over microscope slides of the actual bile duct, peering at the stained
images and trying to figure out what these alien tunnels could be. They
tried a different stain, a trichrome one that colors collagen cobalt.
These stains turned up normal, but modern medical textbooks offered no
advice as to what those odd bright bands were.
What
deepened the mystery was the fact that the structures were
in normal tissues. This wasn’t an oddball disease variant; it was the
baseline normal, appearing in slide after slide of normal tissue. It
seemed to appear consistently, almost mocking its investigators to
frustration with its existence and lack of name.
Theise,
Carr-Locke, and Benias were desperate. The team decided they needed to
get tissue from the viewing scope to the microscope slide as quickly as
possible. They needed a patient having their pancreas removed for a
tumor who’d also have to get part of their bile duct removed as well. If
the endoscope was used on this living tissue, just prior to surgical
removal, they could confirm the presence of the pattern, then quickly
freeze the tissue to preserve the structure as much as possible.
“So
we got patients to agree that before they got their surgery, while
they’re lying there on the table ready for the surgery, we would first
endoscope them” so they could see the reticular pattern in the bile duct
and then quickly take a sample of bile duct. And then? “Take it out and
put it on this little metal platform with this goop we put things in to
do frozen sections, so it makes it hard enough so you can slice really
thin sections,” he explained.
And there it was again: the reticular pattern, this time not through an endoscope, but rather on a slide, under a microscope.
These
slices proved two things for the team. First, they were onto something
that only endoscopists and a liver pathologist could have seen with each
other’s complementary skill set. And second, perhaps more importantly,
they had identified anatomy that no one had described before.
What
is an organ? Anatomy textbooks are rather fuzzy about what defines an
“organ,” requiring one to have primary tissue—parenchyma—and “sporadic”
tissue, called stroma, which can be nerves, vessels, and other
connective tissue. Organs are the necessary building blocks of organisms
(hence, the name), and can be gigantic or microscopic. So long as cells
clump together to form tissues, and these tissues organize themselves
into organs that perform specific functions in the survival of an
organism, that mass of tissues and cells can be called an organ.
Theise,
Carr-Locke, and Benias weren’t sure what to call this space with its
collagen bundles and fluid. The fluid itself appeared rich in proteins
typical of lymphatics and serum, but the space was neither lymphatic nor
vascular (meaning that it contained neither veins nor arteries), so
what could it be?
That’s
when it dawned on them that what they’d stumbled upon was actually
talked about in medical textbooks, but that they were the first to
actually define it.
This
thing they were looking at, struggling to understand with its bizarre
structure and rule-breaking form, was the interstitium, a space vaguely
described in textbooks as where “extracellular fluid” is found, the
fluid that isn’t contained within cells. What doctors had defined as
“dense connective tissue” wasn’t dense connective tissue at all. In
fact, they were all fluid-filled structures that only appeared to be
densely compacted when tissues were made into slides, the fluid draining
away, the collagen lattice collapsing onto itself.
They had a theory—that the space was the interstitium—and a way to prove it. They were on to something.
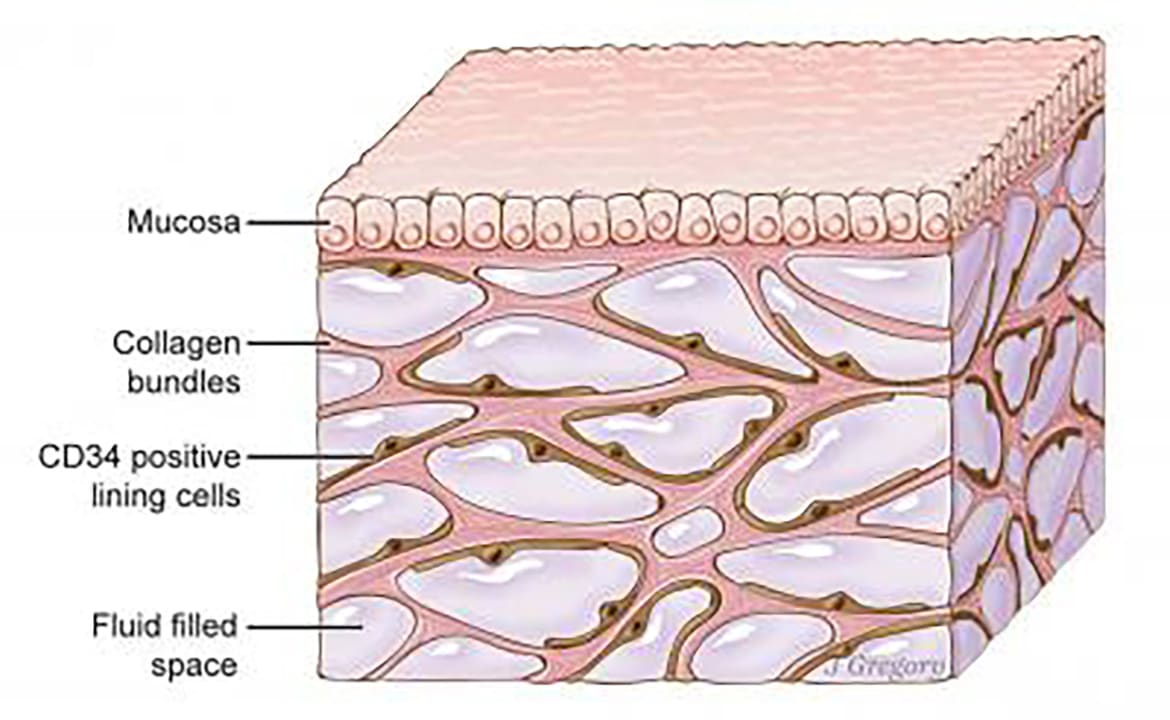
ILLUSTRATION BY JILL GREGORY. PRINTED WITH PERMISSION FROM MOUNT SINAI HEALTH SYSTEM, LICENCED UNDER CC-BY-ND
Newfound 'organ' had been missed by standard method for visualizing anatomy
So
far they had only recognized this in the bile duct. But Theise began to
recognize through his daily lot of diagnostic slides from surgical
resections and biopsies of all sorts of tissues and tumors that the
dense connective tissue layers of other parts of the body also had the
same appearance as this layer in the bile duct. He noticed it in stomach
and intestine and esophageal specimens, then he saw it in fascia around
muscles and in fat. And then he noticed it around veins and arteries.
Then skin.
It
seemed to be everywhere, and Theise realized the potential enormity of
what they’d discovered, calculating that it was largest organ of the
body by volume—larger even than that of skin due to its wrapping around
every organ, including the skin. At about 20 percent of all the fluid of
the body, and about 10 liters, it was gigantic despite the fact that it
could only be seen by peering through a microscope: The cardiovascular
system (heart, veins, arteries, and capillaries) weighed in at about a
third of that volume, the cerebrospinal fluid 20 times smaller.
Neil
Theise’s office at the New York University School of Medicine is
unassuming and cramped. Books are spilling out of shelves; his desk is
dominated by a state-of-the-art microscope. He often works in solitude,
and has a meditative, spiritual streak; the wall opposite his desk
features a photo of him with the Dalai Lama. Behind Theise, outside a
window, lays a mess of rooftops and cars and concrete, with the Empire
State Building rising above it all.
It’s
not a place one would think a major biological discovery was made,
where Theise pushed against disbelievers about his work, suggesting that
he was making something out of nothing, or worse, that the thought of a
new organ snuggled just beneath our skin—right underneath our eyes
despite advances in technology—was preposterous. We’d found all the
organs there possibly could be to be found; how could an organ have
escaped noticed until 2018?
“We
always thought those cracks were, ‘Oh, we tore the tissue a little,’”
Theise said as he flipped through slides that consistently showed the
wavy, almost dancing, spaces that were in each slide. “But no, those
tiny ‘cracks’ are the remnants of the interstitial spaces. For 200
years, we said these cracks were just tear artifacts.”
Theise went further. With organs that contracted constantly, like the gastrointestinal tract or heart,
why was it that they were so flexible, so capable of handling the daily
stress of continuing to contract predictably, automatically, and
regularly without wearing out? “It’s a shock absorber,” Theise realized.
These cells formed a protective, elastic sort of wall around each
organ, allowing them to do their perform pressurized functions that
would otherwise break them down over time. Instead, they’re going on and
on, thanks to the interstitium.
What’s
next for Theise, Carr-Locke, and Benias? They’re bracing for feedback,
but looking forward to the as-yet-unexplored, boundary-pushing potential
of the interstitium. Theise said their team had submitted their paper
to eight different journals (one sending the feedback that a new organ
was “not of interest to a general audience”) before finally being
accepted by Scientific Reports.
“There’s something new here,” he said. “No one’s ever seen it before, but it’s been there the whole time.”
No comments:
Post a Comment