We even now have testing protocols as well
all this means that with just this, we should be able to mitigate all victims to at least some degree, and perhaps even sharply reduce the number of victims before we are finished. great news on this disease.
Over-the-counter antihistamine repairs nerve damage caused by MS
By Paul McClure
https://newatlas.com/medical/antihistamine-reverses-ms-nerve-damage/?
A new study has found direct evidence that an over-the-counter antihistamine can repair the nerve sheath damaged in people with multiple sclerosis
A new study has found direct evidence that an over-the-counter antihistamine can repair the protective nerve sheath that’s damaged in people with multiple sclerosis. The researchers also identified a biomarker that can be used to measure the drug’s effectiveness, opening the door to a potential new treatment for the debilitating disease.
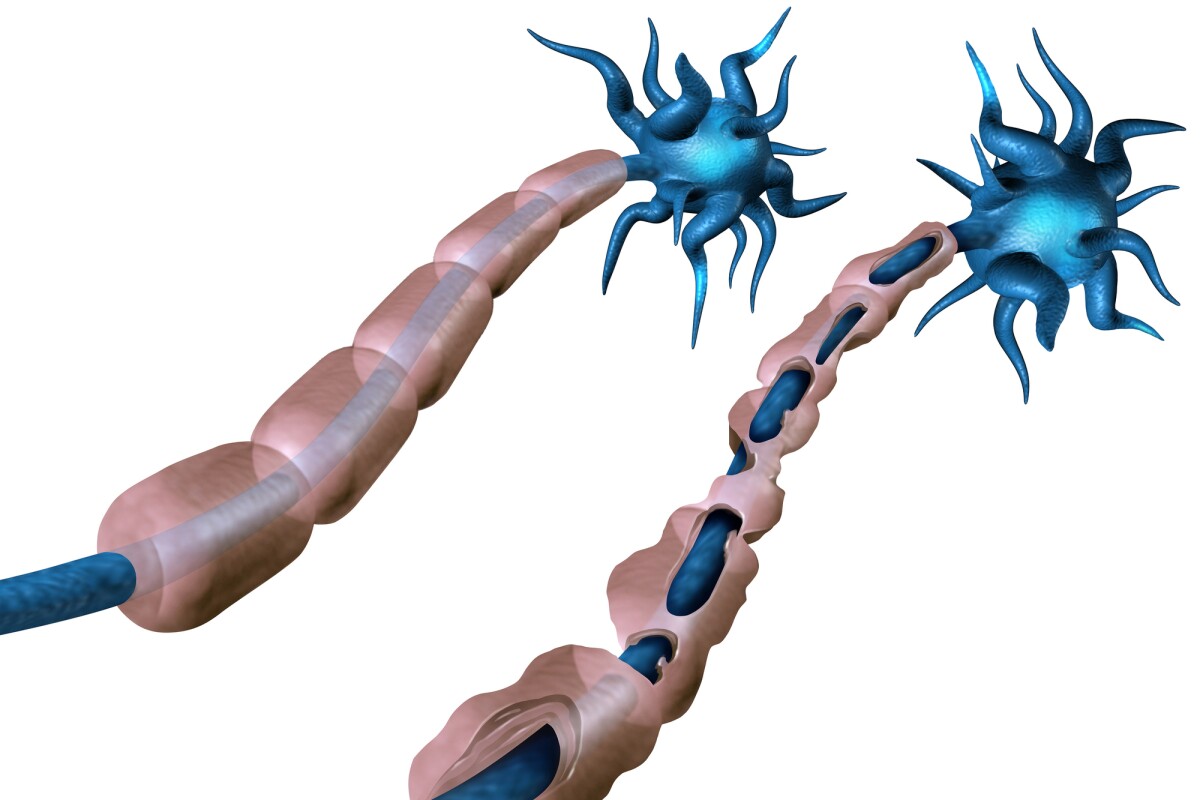
In the autoimmune disease multiple sclerosis (MS), the body’s immune system attacks the protective myelin sheath that covers nerves, causing irreversible damage and disrupting communication between
The goal of any MS treatment is to reverse demyelination, which would return proper nerve function and reduce or prevent long-term disability. Rather than reversing the demyelination process, current treatments focus on the autoimmune aspect of the disease, blocking immune cell access to myelin or otherwise lessening the body’s inflammatory response.
Now, researchers from the University of California San Francisco have identified an over-the-counter antihistamine called clemastine that can reverse damage to the myelin sheath and, what’s more, they’ve identified a biomarker that can measure the drug’s effectiveness.
It all hinges on something called the "myelin water fraction" or MWF. Water that is trapped between the layers of myelin that wrap around nerves in the brain can’t move as freely as water that floats between brain cells. The MWF measures the ratio of myelin water to the brain tissue’s total water content and indicates myelin integrity.
The researchers examined 50 patients with MS enrolled in the ReBUILD trial, who were divided into two groups: the first received clemastine for the first three months of the study, and the second received it only in months three to five and were given a placebo to start. Using magnetic resonance imaging (MRI), they measured the MWF in the patients’ corpus callosum, the thick bundle of nerve fibers connecting the brain's left and right sides that is dense with myelin.
The researchers found that, in the first group, myelin water increased after participants received the antihistamine drug and continued to increase until it was stopped. In the second group, myelin water decreased while they were on the placebo and increased when they took clemastine. The researchers also noted that significant remyelination occurred in areas other than where there were visible MS lesions, that is, areas where the myelin is damaged or scarred.
Based on their findings, they say that measuring MWF changes in the corpus callosum using MRI should be used as a standard biomarker for assessing remyelination therapies.
“This is the first example of brain repair being documented on MRI for a chronic neurological condition,” said Ari Green, corresponding author of the study. “The study provides the first direct, biologically validated, imaging-based evidence of myelin repair induced by clemastine. This will set the standard for future research into remyelinating therapies.”
The study’s findings corroborate the results of a previous UC San Francisco study using the same 50 participants, which found that clemastine reduced delayed nerve signaling.
The researchers say that clemastine stimulates the differentiation of the stem cells responsible for making myelin and provides an alternative way of treating MS that doesn’t focus on the immune system. But, while the results are promising, they say work is still needed to fine-tune the treatment.
“Clemastine can only be partially effective at the doses we can use,” Green said. “It can be sedating, which may be especially undesirable in patients with MS. We are hopeful better medications will be developed, but clemastine has proven to be the tool to show remyelination is possible.”
In the future, the researchers plan to look at clemastine’s potential for treating brain injury in premature infants, who often experience myelin damage.
No comments:
Post a Comment