This is worrying because it implies a continuing impact on victims that does not also resolve quickly.
Too soon for numbers, but it does impact possibly at a threat level not been otherwise detected.
We have heavily over reacted to this disease with strategies that look seriously flawed. We need real detection of the agency for when the main symptoms have already disappated.
New insights into how COVID-19 can impact the brain and CNS
By Rich Haridy
January 12, 2021
New research demonstrates SARS-CoV-2 can directly infect brain cells
VIEW 2 IMAGES
https://newatlas.com/health-wellbeing/coronavirus-infect-damage-brain-neurological-cns-yale/
A robust new study led by scientists from Yale School of Medicine has comprehensively demonstrated how SARS-CoV-2, the novel coronavirus that causes COVID-19, can infect the brain and central nervous system (CNS). The study validates a growing body of observational research attributing neurological issues to COVID-19.
As 2020 progressed and we learned more about the effects of COVID-19, many clinicians began to suggest this novel virus causes more than just respiratory disease. The temporary loss of one’s sense of smell was an early unexpected sign the virus could be affecting parts of the brain. Unlike a common cold, which causes similar symptoms due to simple sinus congestion, COVID-19 seemed to be disrupting this sense in a different way.
From increasing cases of stroke, to memory loss and other cognitive complaints, a number of neurological concerns appeared to suggest the virus was somehow getting into the brain, but how it was doing that wasn’t particularly clear. Studying the effects of SARS-CoV-2 on the brain presented researchers with a challenge. Beyond post-mortem autopsies it is virtually impossible to sample brain tissue directly, so it is difficult to directly investigate whether the virus was explicitly infecting the brain.
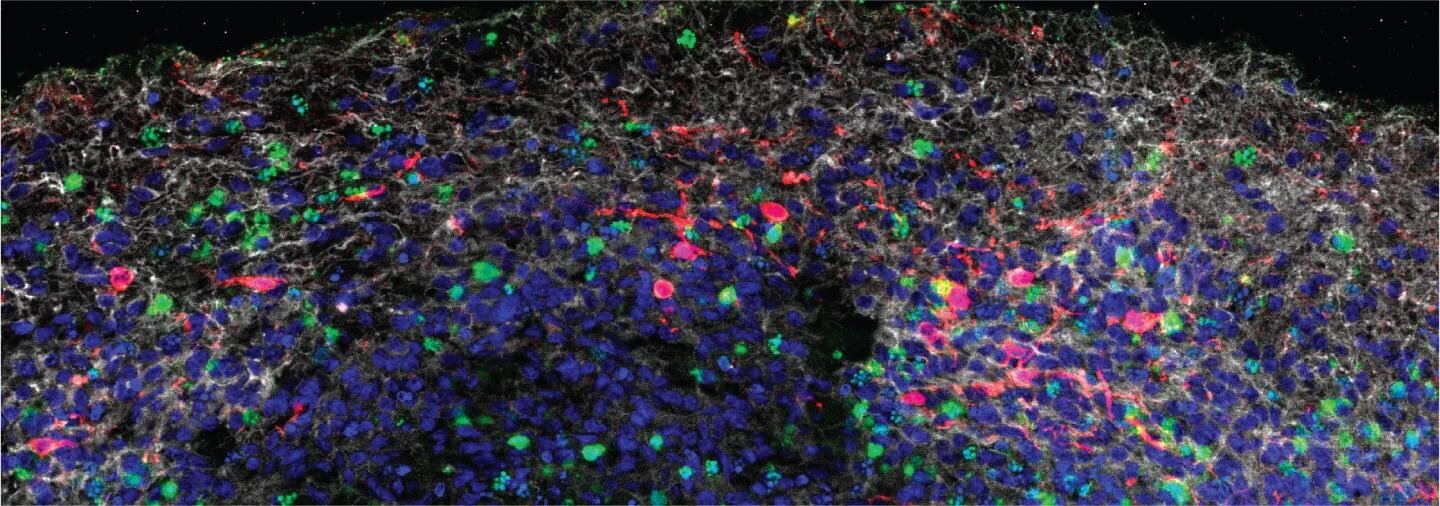
The new Yale-led research utilized a variety of methods to investigate how the virus could infect brain cells. Lab-grown brain cell models called brain organoids, detailed SARS-CoV-2 mouse models, and post-mortem human brain tissue were all aspects of the new study which ultimately discovered the novel coronavirus can indeed directly infect brain cells.
"Our study clearly demonstrates that neurons can become a target of SARS-CoV-2 infection, with devastating consequences of localized ischemia in the brain and cell death," says co-senior author Kaya Bilguvar. "Our results suggest that neurologic symptoms associated with COVID-19 may be related to these consequences, and may help guide rational approaches to the treatment of COVID-19 patients with neuronal disorders."
An image of a human brain organoid shows numerous dying cells (green) surrounding neurons (gray) that have been infected by SARS-CoV-2 (red)
2021 Song et al
The new study offers plausible evidence demonstrating SARS-CoV-2 can infect the brain and central nervous system (CNS), but due to a lack of robust clinical research it is still unclear what those neurological effects of COVID-19 are in the long-term. A recently published review article surveyed more than a century of viral infections and suggests there is a precedent for flu-like viruses leading to neurological complications.
"Since the flu pandemic of 1917 and 1918, many of the flulike diseases have been associated with brain disorders," explains lead author on the review, Gabriel A. de Erausquin. "Those respiratory viruses included H1N1 and SARS-CoV. The SARS-CoV-2 virus, which causes COVID-19, is also known to impact the brain and nervous system."
The review lays the foundation for a new cohort study dedicated to investigating the long-term impacts of SARS-CoV-2 on the brain. The study aims to follow a large volume of COVID-19 patients, with evaluation points at six, nine, and 18 months post hospital discharge.
“Scientific leaders, including the Alzheimer's Association and representatives from more than 30 countries – with technical guidance from the World Health Organization – have formed an international, multidisciplinary consortium to collect and evaluate the short‐ and long‐term consequences of SARS‐CoV‐2 on the CNS,” the new review article explains. “This program of studies aims to better understand the long‐term consequences that may impact the brain, cognition, and functioning – including the underlying biology that may contribute to AD [Alzheimer’s disease] and other dementias.”
A significant volume of questions still remain: How does SARS-CoV-2 get into the brain? What makes a person more susceptible to neurological infection? Are there long-term neurological effects from mild COVID-19 cases? Does SARS-CoV-2 infection increase one’s chances of developing neurodegenerative conditions such as Parkinson’s or Alzheimer’s?
Akiko Iwasaki, an author on the new Yale study, says future work will need to answer all these questions as we begin to grapple with the long-term after-effects of the pandemic. And this Yale study, demonstrating how the virus can infect brain cells, is the first step on the path to finding answers.
"Understanding the full extent of viral invasion is crucial to treating patients, as we begin to try to figure out the long-term consequences of COVID-19, many of which are predicted to involve the central nervous system," says Iwasaki.
No comments:
Post a Comment