This is interesting. Stressed cells can reduce to some form of dormancy with the potential for reversal. Now we are starting to understand working with it.
good item to be introduced.
also a reminder of just how even today we are on the outside looking in. af\\t\er lifetimes of direct informed scientific effort.
Why Do Cells 'Turning Off' Underlie so Many Chronic Diseases?
Understanding the Cell Danger Response is critical for treating treating spike protein injuries and many other complex illnesses
By A Midwestern Doctor
February 3, 2026
When working with chronic illnesses, one of the most common observations is that a “shock” happens to the body, and things that used to function stop working and won’t return to how they were previously functioning due to issues which appear to be at a cellular level. Frequently, these situations are addressed by trying to use integrative therapies to treat the perceived issue (e.g., inflammation, mitochondrial dysfunction or gut dysbiosis), while in other cases (e.g., after a stroke) it’s viewed as irreversible and patients are encouraged to live with it.
I very much believe cells “turn off,” but hold the perspective if you can reverse what caused them to turn off (e.g., interrupted blood flow or a chronic infection) and then give the cells a signal to “turn back on” these conditions can be cured—including many cases where the cells are assumed to be permanently “dead” but in reality are simply trapped in a dormant state.
For example, now and then, I’ve observed a specific treatment for a spike protein injury (severe COVID, long COVID or a vaccine injury) have a rapid effect that was so dramatic it would have been difficult to believe it had happened had I not witnessed it firsthand. Likewise, I have now received hundreds of reports of chronic debilitating issues suddenly “go away” once DMSO was used. Like the COVID cases I witnessed, many of these recoveries are difficult to believe to the point that had I not made a point to compile and present these cases (along with the thousands of studies corroborating these experiences), people would not have believed they could occur.
In turn, throughout my career, whenever I spotted a treatment rapidly restore someone’s vitality, I would always ask “Why did this happen?” and I gradually realized two mechanisms again and again seemed to account for most of the cases where I observed this happen.
The first was that impaired fluid circulation in the body was restored, most commonly by restoring the physiologic zeta potential (something the spike protein is uniquely suited to inhibit). Since this is a complex but relatively unknown topic, I’ve worked to explain what zeta potential is, how its disruption creates illness by impairing fluid circulation throughout the body, and the methods I know of that can restore it.
Note: in parallel to doing this, I also discussed the fourth phase of water (something also critical for the health of the body) as the two concepts are deeply interrelated.
The second, as mentioned before, was that cells had “turned off.” This article will focus on the second, and illuminate what I believe is the best model currently in existence to explain why cells “turn off” and how to turn them back on.
What is the Cell Danger Response?
For cells to survive, something has to protect them from the innumerable threats they encounter. In complex organisms, we typically assign that role to the immune system. In contrast, in single-celled organisms (e.g., bacteria), it’s fulfilled either by them putting protective agents into their environment (e.g., bacteriocins to kill enemy bacteria) or them evolving resistance to the danger they are facing (e.g., antibiotics).
However, those are not the only options.
For example, bacteria are well recognized to form spores in adverse environments, and as I highlighted in this article, a large portion of (mostly ignored) data shows that when bacteria (and certain fungi) are stressed, some survive by changing into completely different morphologies. As these microorganisms often create chronic illness (rather than exist in a non-harmful harmony with the body), many schools of natural medicine advocate for either encouraging them to switch back to the non-pathologic state (e.g., by fixing the body’s terrain) or eliminating them with an anti-microbial therapy which, unlike many common antibiotics, does not provoke the creation of these pathologic bacteria.
Note: one of the most common issues these researchers observed is that classic cell-wall targeting antibiotics (e.g., penicillin) would fail to kill some of the targeted bacteria and instead shift them to cell-wall deficient mycoplasma-like bacteria—which are difficult to detect and provoke chronic inflammation in the tissues they inhabit.
Similarly, one school of thought within oncology argues that cancer results from cells being exposed to lethal or sublethal stressors because to survive, they reactivate primitive survival mechanisms existing within their genome from when they were not a symbiotic part of complex organisms and instead simply voraciously fighting for their own survival in a hostile environment. Like the pleomorphic theory of bacteria, a large volume of evidence exists for this theory (e.g., see this 2024 paper), but sadly it remains relatively unknown and our medical system continues to ignore the necessity of working in harmony with the body to resolve illnesses.
Likewise, when cells are stressed by their environment, they will frequently transform into a more defensive state primarily mediated by the cell’s mitochondria (which are essentially bacteria and able to rapidly adapt to changes in their environment). This process has been observed by many (e.g., some call it the integrated stress response), and I believe the process is the most comprehensively described by the Cell Danger Response (CDR).
The CDR concept is frequently credited to Robert Naviaux who integrated all of the existing scientific knowledge on cellular adaptations, utilized a variety of established approaches (e.g., genomic analysis), and, most importantly, used an innovative but relatively unknown diagnostic method, metabolomics, to map out the CDR.
Metabolomics uses mass spectrometry to identify every biomolecule present in a sample of blood, which is both quite feasible and provides an in-depth understanding of the body which, to my knowledge, cannot be obtained with any other existing technology (e.g., the endless lab tests that provide a narrow snapshot of the body which may not have any correlation to the patient’s symptoms). This is how Naviaux described the merits of the technology:
First, fewer than 2,000 metabolites constitute the majority of the parent molecules in the blood that are used for cell-to-cell communication and metabolism, compared with 6 billion bases in the diploid human genome. Second, metabolites reflect the current functional state of the individual. Collective cellular chemistry represents the functional interaction of genes and environment.
Note: at the time Naviaux pioneered this approach, AI systems which could analyze large packets of metabolic data to discern subtle patterns did not exist. After I first broached this topic in a 2023 article, LLMs came into widespread use, and numerous parties have used them to build upon the patterns Naviaux recognized (e.g., see this, this, this, and this paper) and likewise, other teams have mapped out how metabolomic patterns (mirroring the CDRs) underlie key inexplicable chronic illnesses like chronic fatigue syndrome and fibromyalgia.
The process of the CDR essentially is as follows:
1. Something stresses the cell.
2. Mitochondria within the cell rapidly detect this stress (e.g., before the stressor can kill the cell). This detection, Naviaux argues, is due to electrons that previously were available to mitochondria being diverted to the stressor (e.g., an invading virus hijacking the cell to reproduce, a heavy metal being present, or many of the harmful [electron stealing] chemicals we are exposed to now), which creates a voltage drop in the mitochondria.
3. The mitochondria then reduce or terminate their primary function (creating energy in the form of ATP for the cell) and switch from an anti-inflammatory to a pro-inflammatory state (macrophages also switch from an anti-inflammatory to a pro-inflammatory form).
4. Because the mitochondria producing ATP uses up a lot of oxygen, once that production is reduced (or becomes incomplete) and the mitochondria shift to producing different biomolecules, the available oxygen in a cell rapidly increases. For context, mitochondria contain ≈1,500 proteins tailored to meet the needs of each cell type and catalyze over 500 different chemical reactions in metabolism.
These mitochondrial effects (particularly the elevated oxygen) cause the following to occur:
•Production of complex proteins (polymers) is reduced, which viruses require to reproduce.
•Protective changes in the behavior of the whole organism (e.g., increased tiredness that induces the sleep needed to facilitate healing or a desire to isolate so the infection is not transferred to other members of their group).
•Antiviral and antimicrobial substances are released inside the cell.
•Warning cells in the vicinity that a danger is present.
•Increased consumption (autophagy) of components within the cell, including the defective parts of the mitochondria and the mitochondria themselves.
•Changes in gene expression and mobilization of parts of cellular DNA.
•The cell membranes stiffen so things are prevented from passing through it.
Note: a long time ago, a mentor versed in some of the most remarkable forgotten sides of medicine showed me an ancient test his teacher used to evaluate if the body was consuming oxygen properly (something they believed was critical for proper health). The test was known as the blood crenation test and assessed the degree to which cells would change their size once placed in a hypertonic solution. After I learned about the CDR, I realized that the test detected if the membranes had stiffened due to an active CDR and mitochondria, in turn, not correctly consuming oxygen. That stiffening is greatest during CDR1 and begins to soften during CDR3 (explained below). I found this fascinating because the therapy (designed to treat numerous illnesses through restoring the oxidative metabolism of cells) he used the blood crenation test for had two stages of treatment, and the second stage could only be used once the first stage had sufficiently softened the cell membranes.
In the previous article on zeta potential, I argued that a key reason for why zeta potential disruption has become a root cause of so many illnesses is due to the physiologic mechanisms for maintaining zeta potential having evolved in an era where the human body faced far fewer zeta potential disrupting toxins. Because of this, the baseline zeta potential (charge) our body is designed to maintain is often not strong enough to counteract those harmful environmental influences.
The CDR likewise evolved in an era when humans faced far fewer stressors and is not appropriately calibrated for the modern world. For example, when the CDR is activated, the oxidizing environment causes cells to sequester rather than excrete heavy metals. This is a problem since heavy metals (which are now common in our environment) are both a common cause of chronic illness and a trigger for the CDR.
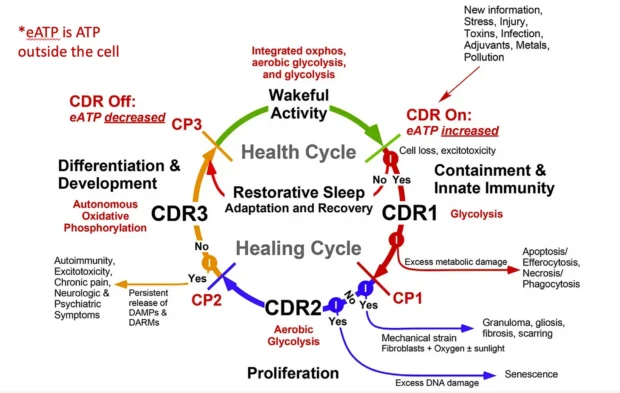
When Naviaux originally mapped the CDR out, he thought that it had one phase, but in time realized it had three different phases, the initial response, a proliferative phase (which rebuilds tissue), and then the cell beginning to return to its initial function:
Naviaux’s central argument is that while the CDR is a normal adaptive response, it will create problems if cells get stuck in one of the CDR phases because they did not receive the final all-clear signal to exit the CDR.
Additionally:
• Chronic diseases are characterized by impaired communication between cells and tissues. If this occurs at a young age (e.g., in autism), the normal trajectory of development is altered, leading to the abnormal tissue and organs the body’s systems must adapt to. In adults, these alterations cause tissue and organ performance to degrade over time, eventually leading to various problems such as cancers and organ failures.
• During CDR2 (which, among other things, Naviaux links to cancer), dividing and migrating cells cannot establish long-term metabolic cooperation between cells because their location within tissues is continuously changing. CDR3, in turn, is the integration phase that allows cellular communication to be restored, and hence is critical to complete for many complex illnesses.
• Additionally, CDR3’s completion is aided by the autonomic nervous system being in a rest and recovery state (facilitated by the vagal nerve—the parasympathetics are one of the foundational ways to communicate safety to the body). My colleagues believe this helps to explain why the converse, excessive stress, and sympathetic activity that characterizes the modern age can have such a large impact on chronic illnesses, as they signal to the body danger (that requires a CDR) is still present.
Note: I do not believe the CDR is the only dysfunctional cycle cells enter, but I frequently refer to it because (thanks to Naviaux’s work) it is the most well-mapped-out one. As such, I frequently state I am “treating the CDR” when in reality I believe I am treating something similar to the CDR that responds to treatments similar to those which treat the CDR. For example, I believe one of the key issues which underlies many diseases are cells, due to a shock or chronic loss of nourishment, no longer dividing (which fits within the CDR framework), but many of the cases where I’ve seen this happen do not appear to follow the CDR cycle Naviaux laid out.
What are the effects of the CDR?
Naviaux published a few key papers which elucidated the CDR. They are as follows:
• The original 2014 paper which explained the CDR.
• A 2016 study of patients with chronic fatigue syndrome (CFS) identified consistent patterns within their metabolomics. Those hypometabolic changes resembled dauer, an evolutionarily conserved state organisms enter that makes them much more capable of surviving environmental stressors and conserving energy but much less able to engage in normal activity (e.g., a functional life free of suffering and disability). Since the biological clock within those cells slows (and they can survive periods of resource starvation), they can outlast the cells that fail to make this transition and take over once conditions are safe for the cells to return to normal.
Note: many of the genes involved in dauer have been actively studied for promoting longevity (e.g., they overlap with the changes created through caloric restriction). Additionally, in dauer, behavioral responses become “brittle,” such that small stimuli produce significant responses in otherwise docile animals, a phenomenon also commonly observed in complex chronic illnesses.
• A pilot 2017 study where autistic children were provided a CDR blocking agent. This double-blind trial demonstrated significant improvement in autistic children, which to my knowledge, has not been obtained in any other clinical trial attempting to treat autism.
• A 2017 review of the CDR and the potential applications in using CDR targeting agents for conditions such as autism.
• A 2018 paper discusses the CDR’s three stages and how they are part of the body’s normal healing cycle. This is the most detailed overview of the CDR Naviaux has written and the paper I most recommend interested parties reading.
• A brief 2020 paper connecting the CDR to mitochondrial dysfunction and chronic illness.
• A 2020 study evaluated the link between viral infection and the CDR. It found the HHV-6 virus (to which 90% of the population is exposed by age three) could trigger the CDR. Once activated, the CDR shielded cells from other viruses as there was up to a 99% decrease in their infection from influenza or HSV-1. Notably, the CDR persisted even when HHV-6 was almost undetectable, and serum from CFS patients could induce the CDR within healthy cells (and matched the CDR seen in CFS), thus demonstrating that a pathologic CDR can persist long after the inciting stimulus disappears.
• A 2021 study exposed rats to the primary CDR-inducing agent (ATP) and then measured the metabolic and behavioral changes that followed (e.g., whole body oxygen consumption decreased by 74% and rectal temperature dropped by 6.2˚C in 30 minutes—both of which are massive changes). This paper is the most detailed published study (I know of) that has been conducted on how the CDR alters both behavior and biochemistry (over 200 metabolites from 37 different biochemical pathways were changed). Furthermore, it found that most of the changes returned to baseline in a few hours and that the responses in male and female rats to ATP were noticeably different (males were more sensitive to behavioral changes, females were more sensitive to metabolic changes).
• A 2023 review paper that discussed the current understanding of the CDR and methods for treating it. Much of that paper is discussed in this article on treating the CDR.
• A 2025 review paper (his most current work) proposing that autism results from being genetically prone to mitochondrial sensitization (or intracellular calcium signaling to environmental change), plus early exposure to environmental triggers that activate metabolic features of the CDR and recurrent or persistent exposure to CDR-activating triggers for at least 3–6 months during the critical neurodevelopmental window.

No comments:
Post a Comment