What is obviously true is that our understanding of pain has been mostly naive forever. here we are now discovering the rest of the story almost for the first time. Are we really that ignorant?
A whole lot of biology remains Terra Unknown even with a full press investigation for centuries even.
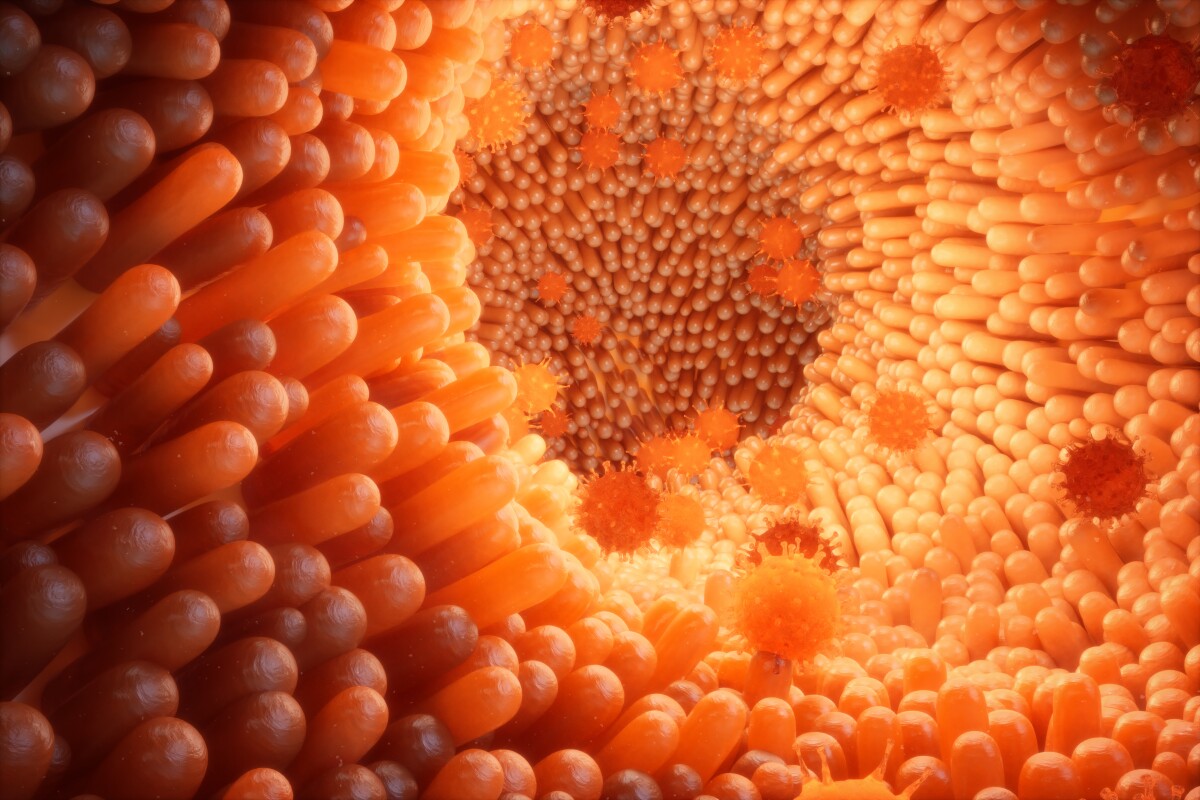
Studies uncover anti-inflammatory role of pain-sensing gut neurons
By Rich Haridy
October 16, 2022
Two studies uncovered new ways pain-sensing neurons in the gut can trigger processes that protect from inflammation
https://newatlas.com/science/anti-inflammatory-pain-sensing-gut-neurons-microbiome/
A pair of new studies published in the journal Cell have reported on unexpected ways pain-sensing neurons in the gut can serve as more than just sensory alarm systems. The research suggests these neurons also can directly protect the gut from inflammatory damage.
“It turns out that pain may protect us in more direct ways than its classic job to detect potential harm and dispatch signals to the brain," said Isaac Chiu, senior investigator on one of the two new studies.
Chiu's work, alongside a team from Harvard Medical School, was focused on the ways pain neurons in the gut communicate with goblet cells, a type of cell that lines the intestine and secretes protective mucous in the presence of inflammation. While it was known that there must be some way these pain-sensing neurons communicated threats to other gut cells, until now scientists didn't understand exactly what mechanisms were at play.
In the Harvard-led study, the researchers discovered goblet cells carry specific receptors that pick up signals sent out from pain neurons. When pain neurons are stimulated they release a chemical called calcitonin gene-related peptide (CGRP). And this chemical signal looks to be a key instigator of goblet cell mucous secretion.
Across several mouse experiments the researchers demonstrated how general gut health is maintained by CGRP secretion from pain neurons. Not only were goblet cells activated by CGRP in the presence of acute inflammatory pain or damage, but in a healthy gut there seemed to be microbes triggering this process as a way of maintaining microbiome balance.
“This finding tells us that these nerves are triggered not only by acute inflammation, but also at baseline,” Chiu explained. “Just having regular gut microbes around appears to tickle the nerves and causes the goblet cells to release mucus.”
One compelling implication from these findings is that systemically suppressing a body's pain response could potentially have detrimental effects on this protective mechanism. When the researchers looked at mice engineered to either lack pain neurons in the gut or lack CGRP receptors they saw greater inflammatory damage.
“In people with inflammation of the gut, one of the major symptoms is pain, so you might think that we’d want to treat and block the pain to alleviate suffering,” noted Chiu. “But some part of this pain signal could be directly protective as a neural reflex, which raises important questions about how to carefully manage pain in a way that does not lead to other harms.”
A second recently published study, this time led by scientists at Weill Cornell Medicine, also reported finding a new protective function in pain-sensing gut neurons. This research focused on gut nerves with a specific kind of receptor dubbed TRPV1.
When TRPV1 receptors on gut neurons are stimulated, the brain responds with by generating a burning kind of stomach pain that anyone with an inflammatory bowel condition would be familiar with. However, somewhat counter-intuitively, the researchers found that completely silencing TRPV1 receptors in mouse models led to increased gut inflammation.
So it was clear this pain-sensing response was doing something more than just reporting sensations to the brain. Further mouse investigations revealed the increased inflammatory damage in TRPV1-blocked animals was linked to significant changes in gut bacteria populations.
Turns out TRPV1-expressing gut neurons secrete a molecule called Substance P, and that molecule promotes a healthy balance of bacteria in the gut. The negative effects on gut bacteria when blocking TRPV-1 in mice could be reversed by directly giving the animals Substance P. And, just like in the Harvard study when bacteria were found to "tickle" gut nerves and generate the release of protective mucous, this research found some bacteria could directly activate the secretion of Substance P from gut nerves.
Both of these studies certainly raise a bunch of new questions interrogating the role of gut neurons in inflammatory disease. For example, could future anti-inflammatory treatments target these gut neuron mechanisms?
According to senior author on the Weill Cornell study David Artis, these new findings should change the way we think about inflammatory disease.
“A lot of current anti-inflammatory drugs work in only some patients, and pharma companies really haven’t known why,” Artis said. “Maybe it’s because, when it comes to chronic inflammation, we’ve been seeing only some of the picture – and now the rest, including the role of the nervous system, is starting to come into focus.”
No comments:
Post a Comment