what this does inform is that is that some mental illness is driven by chemical toxins that impact the blood - brain barrier. Cerrtainly aurism has that connection.
This actualy makes a lot of sense because brain tissue is highly protected and really different.Research needs to focus on that barrier as schizoid behavior is also a likely candidate as well.
What i am saying is that the pattern of clues point firmly at the blood brain barrier ,possdibly for all mental illness.
New Cases of Mental Disorders Emerged after Vaccination; 3 Natural Ways to Improve Symptoms
As of early July 2022, 66 percent of the world’s population has been vaccinated with the COVID-19 vaccines. As more people are getting vaccinated, reports on adverse events and even side effects continue to emerge. Not only injuries on vital organs have been reported, but also psychiatric disorders have been reported as well. As off today, there are a total of 10 pieces of medical literature that have reported cases of newly developed mental illness after the patients were inoculated with the COVID-19 jabs.
New Psychiatric Disorders Appeared in Healthy Individuals Following Vaccination
A literature review published in May 2022 in Asian Journal of Psychiatry has reviewed 11 cases of psychiatric reactions to either mRNA or vector-based COVID-19 jabs. The original article mentioned 14 cases, and after a review 11 cases were confirmed with psychiatric disorders and three less relevant cases were excluded.
Four cases were female, six cases were male, the remaining one was not reported. The typical case was commonly a young or middle-aged adult. The average age was 40 years.
Of these 11 cases, there were five cases of psychosis. Three cases reported with altered mental states characterized by disorientation, hallucinations, and labile affect within as early as a few hours up to 10 days of vaccination. Two cases had mania and one had depression.
More than two-third of the adverse events followed receipt of the first vaccine dose. Symptom onset was as early as a few hours up to 10 days of vaccination in all cases.
Almost half of the psychiatric manifestations reported were following administration of the Oxford-Astrazeneca vaccine.
In our view, based on the fact that the majority of the cases were without past history of psychiatric illness before vaccination, and the close temporal relationship to the jabs, the causal relationship between the vaccination and psychiatric disorders are possible.
Below are two examples of representative cases.
In October 2021, a report was published in the journal Psychiatry Research. The report was co-authored by experts from the Department of Psychiatry and Behavioral Health at Stony Brook University in New York and the Northport Veteran Administration Medical Center in New York.
The report describes a 31-year-old single Hispanic male who had no history of psychiatric disorders. After receiving his first dose of an mRNA COVID-19 vaccine, he developed bizarre and inscrutable behavior. Specifically, he became anxious, vigilant and pompous, and also experienced hallucinations. He even mistook a colleague for his lover and talked to himself in his hospital room, saying that an EEG machine in the hospital was communicating with him.
Three weeks later, the man received a second dose of the vaccine, and his symptoms deteriorated significantly.
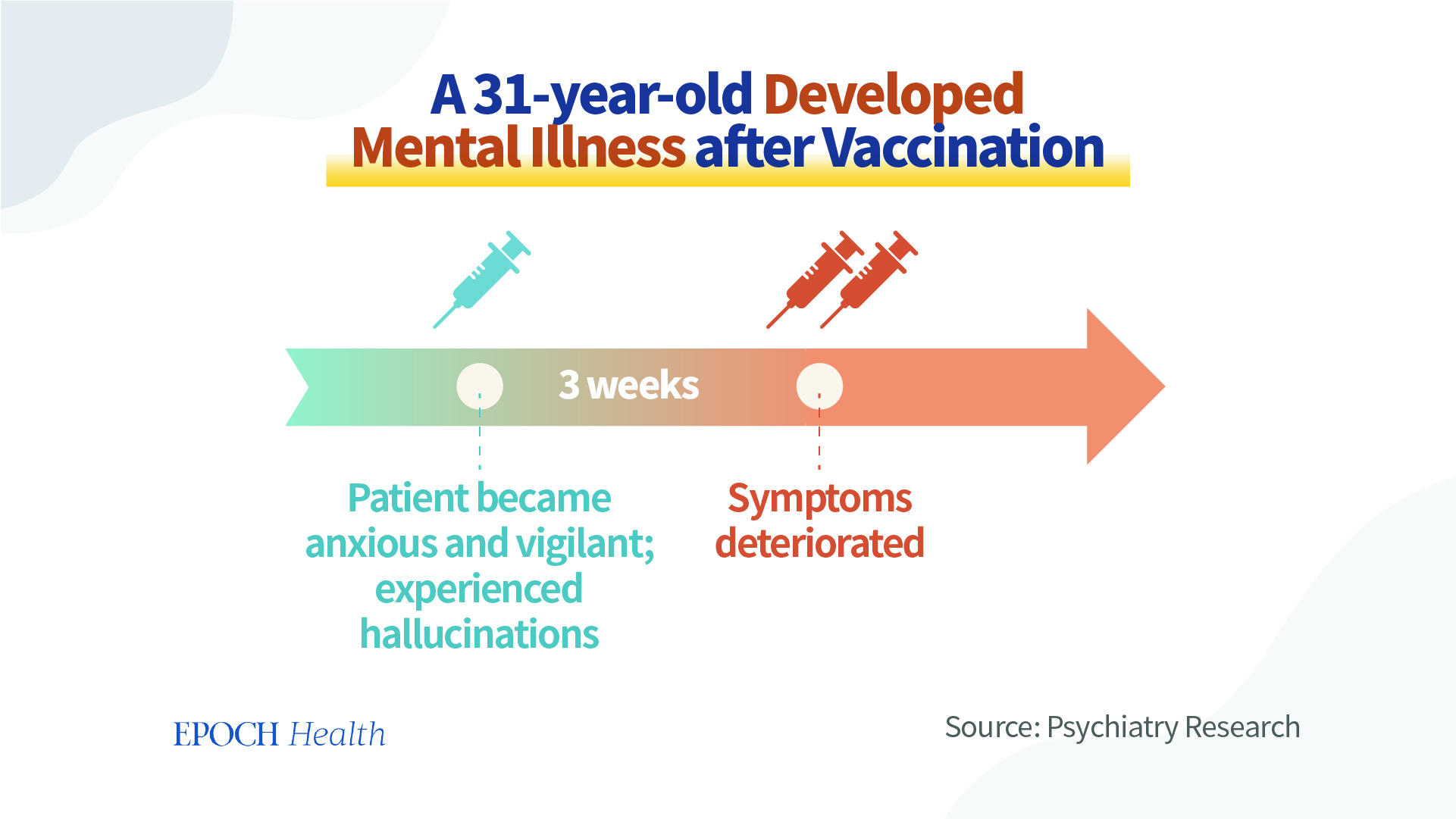
This case shows the correlation between the onset of the illness and the dose and timing of the vaccination. This suggests a causal relationship between this patient’s psychiatric symptoms and the vaccination.
There was another case of psychosis induced by a non-mRNA vaccine.
In this case, the patient is a 51-year-old white male with no history of psychosis or neurodevelopmental delay, and no family history of mental illness. He had lived his early years in a loving and supportive family environment and experienced no major trauma. He has a resourceful personality, a successful career, and a stable long-term partner.
This man received his first dose of the AstraZeneca (AZ) vaccine in mid-March 2021. A few days later, he developed flu-like symptoms and a severe “splitting” headache—a feeling that he had been divided into several individuals.
Ten days after the vaccination, his wife observed that he was experiencing cognitive impairment, feeling confused in time and place, unable to write anything meaningful, and having auditory hallucinations. His behavior changed strangely, and he even stopped eating, drinking, and communicating. So, he was taken to the emergency department by ambulance. His CT head scan and routine blood tests showed no abnormalities, and he was subsequently transferred to the psychiatric unit.
No other cause of illness was found, and the interval between his vaccination and onset of psychosis was short. Subsequently, the patient’s symptoms resolved on their own without the use of psychotropic medication. Therefore, it was tentatively determined that this patient’s psychiatric illness was induced by the COVID-19 vaccine, and the possibility of autoimmune encephalitis was not completely excluded.
What Are the Possible Causes of Psychosis After Vaccination?
The term “new onset psychosis” refers to the first occurrence of psychosis in a patient who has no previous history of psychosis. Both of the aforementioned cases are new onset psychosis, and their onset of illness was very close to the time of vaccination, so there is a strong possibility that their onset of illness is causally related to the vaccination.
Why could vaccines cause new onset psychosis?
First, the SARS-CoV-2 virus can cause a strong immune response in the body, which releases large amounts of inflammatory cytokines that may damage the structure and function of nerve cells and increase the risk of psychosis
In a review published in the European Journal of Neurology in 2021, among a total of 129,008 patients with COVID-19 infection in 23 studies, 138 people with encephalitis (inflammation of the brain) were identified.
In these patients, the average time from their diagnosis of COVID-19 infection to their onset of encephalitis was 14.5 days, with a morbidity rate of 0.2 percent and an average mortality rate of 13 percent. The common symptoms of encephalitis include loss or decreased level of consciousness (77.1 percent), altered mental state (72.3 percent), seizures, headaches, and weakness.
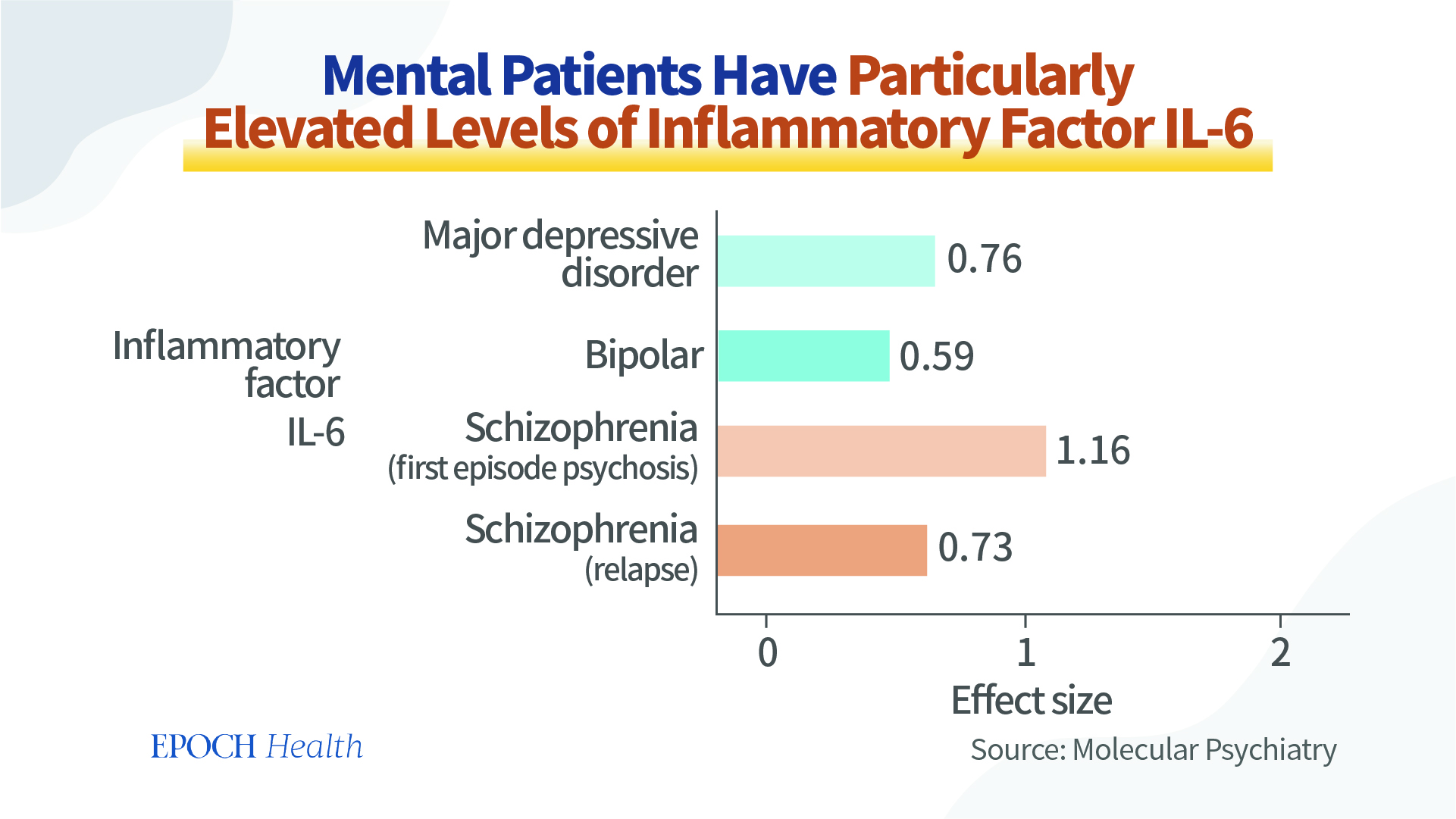
A 2016 meta-analysis published in Molecular Psychiatry pointed out that patients with psychiatric disorders have common characteristic changes in blood cytokines, which are particularly high levels of the inflammatory factor interleukin-6 (IL-6) in the blood during acute seizures.
The pathogenicity of the virus at the beginning of the COVID-19 pandemic was high, and all current vaccines against COVID-19 were designed based on the old virus.
Meanwhile, the spike protein could trigger the chronic inflammatory status so as to impair mental function.
The pathogenicity of the current virus strains has been significantly reduced. And therefore, in this case, we recommend that authorities rationally weigh the benefits and risks associated with the vaccines.
Why Does the Human Mind Have ‘Pathological Changes’?
It is easy to understand that the human organs can have pathological changes. However, why does the human mind also have “pathological changes” when it is invisible and impalpable?
In fact, matter has many molecular levels. Our human body also has many layers upon layers, including molecules, atoms, electrons, quarks, neutrinos. Physicists also admit frankly that they have not fully understood what the tiniest matter is so far.
So, since physicists can’t give a precise definition of what matter really is, how can we arbitrarily say that human spirit does not belong to the scope of matter or substance?
In fact, the human mind is a very subtle substance. Although it’s invisible to the naked eye, much scientific evidence has proven that the mind has shared common properties with other visible or palpable materials.The mind or spirit can be detected by instruments
Modern science has discovered that brain wave recorders can detect the human mind and thought. The mind and thought have also been applied to brain control technologies.Our thoughts can be sensed by others
There is telepathy among family members and friends. And when people send forth kind thoughts, they can be sensed by others.The personality can be remembered and transferred by the organs
According to Freudian psychoanalysis, many mental illnesses are related to traumatic memories from childhood, which are stored in the body’s cells and affect a person’s personality and emotions in adulthood.
So, if the mind is not a substance at all, how can it be remembered by the body’s cells?
In addition, organ transplant recipients often experience personality changes, taking on the traits and talents of the deceased organ donor.
Gary Schwartz, a psychologist and professor at the University of Arizona, has documented 74 cases of heart transplantation and found that 23 of these heart transplant recipients had acquired some of the characteristics of their donors.
For instance, a 47-year-old Caucasian male developed an interest in classical music after receiving a heart transplant from a violinist, and a retired manager who could not paint previously suddenly developed a talent for art after receiving a heart transplant from an artist. Doctors describe these phenomena as “cellular memory.”
An article published in 2020 in the journal Medical Hypotheses discussed the effects of heart transplantation on personality changes and explored the reasons why recipients acquire personality traits of their donors. The article mentioned four types of personality changes that may occur in the organ recipient: changes in preferences, changes in emotions and temperament, modifications in identity, and memories from the organ donor’s life.Psychiatric diseases can be inherited
Psychiatric patients often have a family history of specific genetic mutation loci that can also be passed down from generation to generation.
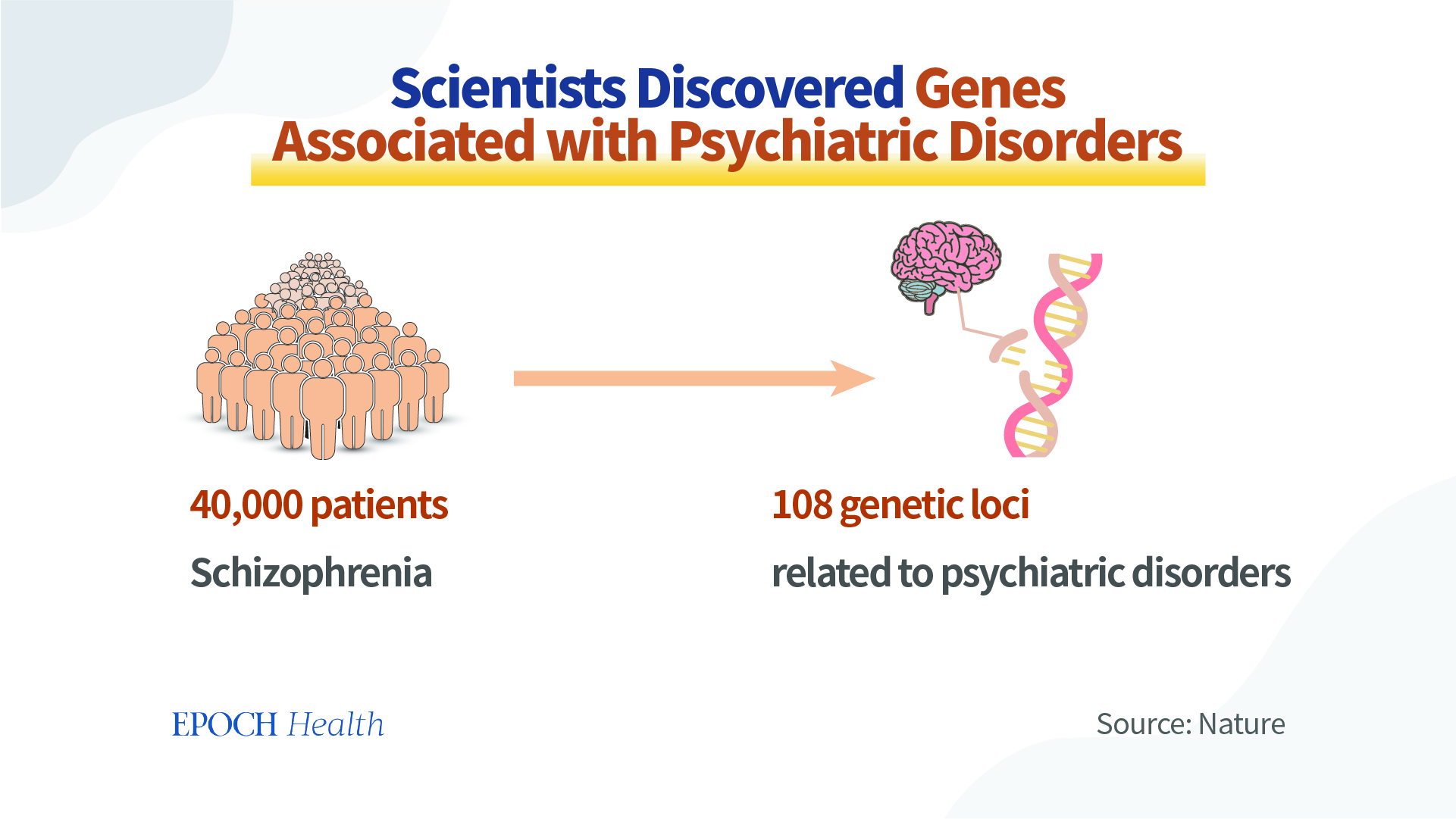
In 2014, a study was published in the journal Nature. The Psychiatric Genomics Consortium (PGC) completed this study of comparing nearly 40,000 patients with psychosis (schizophrenia) to 110,000 people, and found 108 genetic loci significantly associated with psychiatric disorders.
A study published in the European Archives of Psychiatry and Clinical Neuroscience found that schizophrenia has a highly significant genetic component; and the closer the relatives, the greater the effect.
For example, if one of a pair of identical twins has a mental illness, the probability of the other having the illness is 44.3 percent.
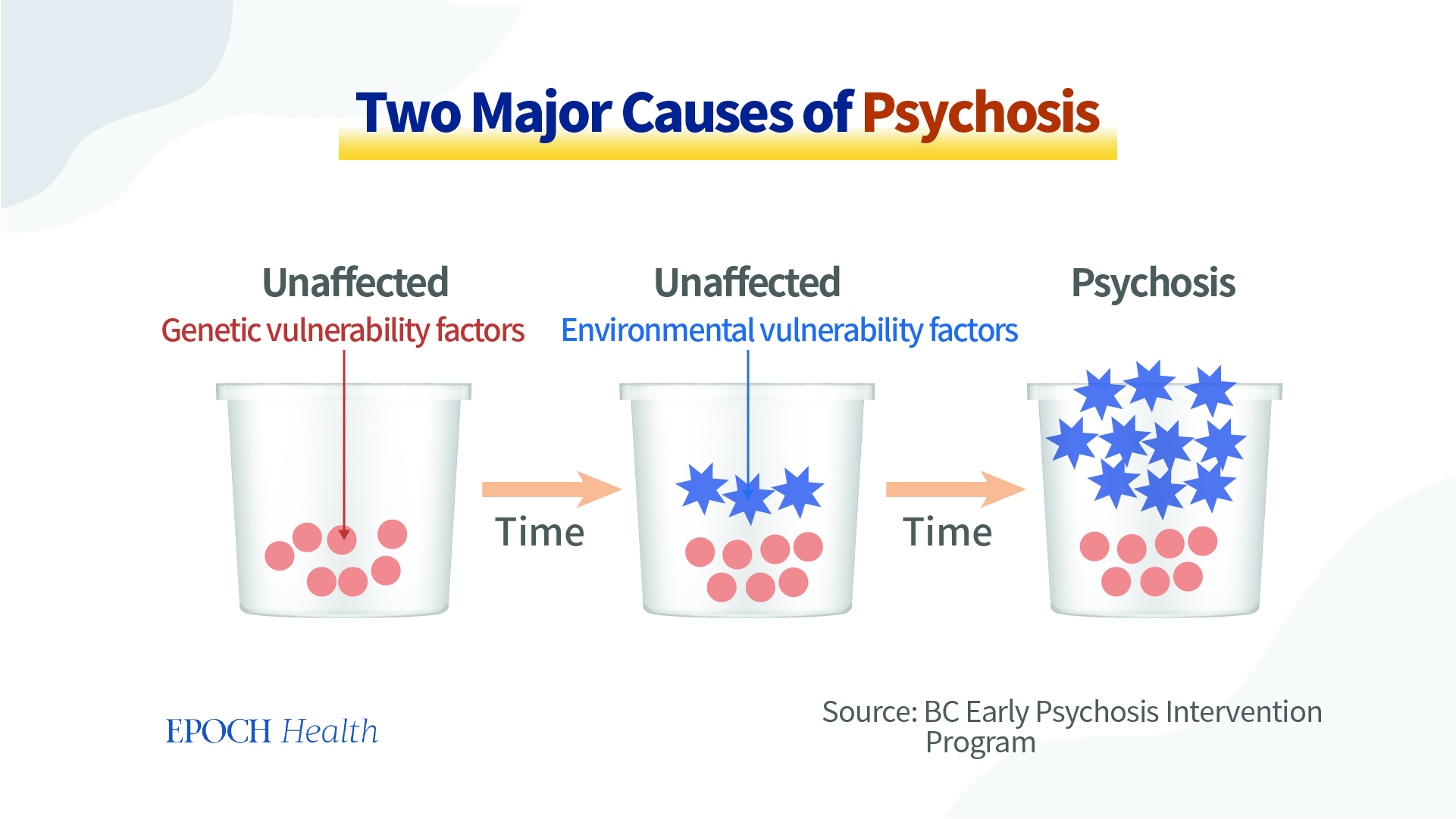
However, on the other hand, even identical twins, who share the same genome, have a probability of less than 50 percent to both develop the disease, suggesting that schizophrenia is not entirely determined by genes. In addition to genetics, schizophrenia is also associated with many hereditary and environmental factors, as well as more subtle ones.
The genetic nature of psychiatric disorders indicates the molecular basis of spiritual phenomenon and spirit could be influenced by the molecular level activities inside our bodies as well.
There are Both Conventional and Holistic Ways to Improve and Treat Mental Illnesses
Since patients with schizophrenia have no physical pathology and only problems on the mental level, doctors have very limited medications at their disposal. These patients require special care not only on a biological level, but they also need a psychological, societal, and holistic treatment plan.Avoiding triggers
All illnesses are the result of a combination of internal and environmental factors. Mental disorders are no different, as people with genetic defects are more likely to be triggered by negative external influences than the general population. Therefore, they need to avoid triggers.Taking medications
Dopamine is a neurotransmitter responsible for excitement in the brain. Modern medicine suppresses the maniac symptoms of schizophrenia by forcibly blocking dopamine receptors with drugs. However, prolonged use of medications may cause drug resistance and eventually lead to refractory psychosis. In view of medications’ limitations, we need to consider other therapies.
Psychotherapy
In psychotherapy, the patient learns to deal with his or her emotions by improving the way he or she looks at things through dialogues and other means.
Electroconvulsive therapy
Short-term electrical stimulation of the brain induces a broad discharge of electricity from the cerebral cortex, restoring normal brain function. This may sound unbelievable, but there have been successful cases.
In fact, the spirit of psychiatric patients may be too weak. If the doctor in the psychiatric hospital just waved an electric baton to them, they would immediately regain his energy because of the reason that he was afraid of being shocked. Therefore, it is necessary to strengthen the main consciousness, the true self, of the psychiatric patients.
In addition, there are natural ways to help patients with mental illness recover faster. For instance, there are ways to make changes on a spiritual level, to get in touch with mentally healthy people and things, including books, literature, and music, to develop a positive outlook on life, and to build self-confidence. Here are some of our recommendations:
Selfless love
The selfless care and love from family and friends is an important force in helping patients recover.
In a popular and familiar example, the recovery of Nash’s schizophrenia, the math genius of the movie “A Beautiful Mind,” was largely due to the love and care of his wife Alicia, who is a beautiful and strong woman. When her husband suffered from schizophrenia, she remained by Nash’s side. Although she could not take responsibility for her husband’s behavior in the illusory world, she took care of him with compassion and responsibility. Such noble, unselfish love has helped Nash finally overcome his mental illness.
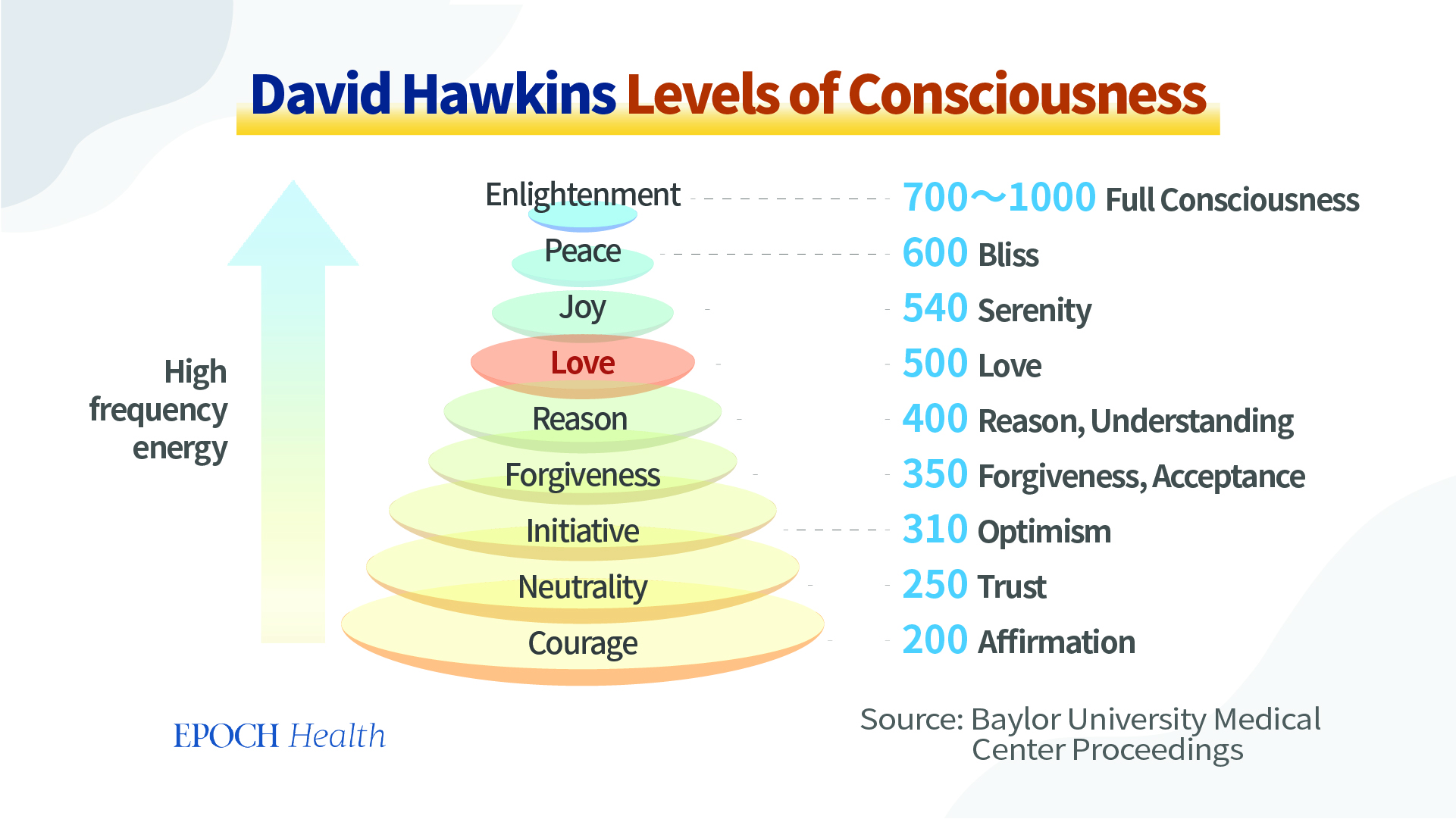
David R. Hawkins, an American psychiatrist, has described the levels of consciousness of the human body. According to him, selfless love, unconditional love, and beneficent love carry a very powerful positive energy, which is a force that has healing power.
In addition, frequent communication with kind, sensible, and strong-minded people is beneficial to the people with a weak mind.
Horticultural therapy
A well-known professor suffered from depression when she was young. At that time, she searched for renowned doctors to treat her illness, but with no success.
Her father, who loved his daughter very much, read about a study that stated that green plants could help cure depression and relieve the symptoms, so he took his daughter to a potted plant exhibition and bought many potted plants. He let her talk to the plants, after which her symptoms were reduced day by day, and she was cured two years later without the use of medication.
This “green miracle” is still mentioned by their family and friends. And this proves that nature and art not only soothe the heart, but also cure illnesses.
In a study published in the journal Complementary Therapies in Medicine, 20 maladjusted elementary school students participated in three gardening activities, including flower arranging, planting, and flower pressing. It was discovered that their salivary cortisol levels decreased by at least 37 percent compared to their pre-participation levels.
Studies have shown that serum cortisol levels are significantly elevated in patients with schizophrenia and gradually decrease after psychiatric treatment, suggesting a negative correlation between cortisol levels and psychiatric illness. The ability of gardening activities to reduce cortisol levels suggests that gardening has an ameliorative effect on mental illness.
Nutritional therapy
The World Federation of Societies of Biological Psychiatry (WFSBP) and the Canadian Network for Mood and Anxiety Treatments (CANMAT), a team of psychiatrists and clinicians from 15 countries, have extensively analyzed the therapeutic effects of nutritional supplements on human psychiatric disorders and found that some nutritional supplements can treat schizophrenia. In descending order of effectiveness, they are:
Methopterin
N-acetyl-L-cysteine (NAC)
Vitamin D
Omega 3 fatty acids (not therapeutic, but can prevent risk factors from turning into psychosis)
In the future, as people continue to update their understanding of the mind and the unknown, there may be more insights into the human body, life, and matter, and more ways to treat and control mental illness will become available.
References

1 comment:
This article is very much helpfull and i hope this will be an useful information for the needed one. Keep on updating these kinds of informative things
Post a Comment