The hard truth is that an injured brain can and will heal slowly. i personally survived twenty minutes without a heart beat but with CPR sloshing blood about.
So realistically after several days it is likely appropriate to withdraw intubation to allow the autotonic nervous system to do its job. Failure then strongly suggests it was impossible. Declaring dead after three days needs way more evidence that that the brain is clearly hibernating.
We obviously need way better diagnostic tools here before we run around declaring someone is brain dead.
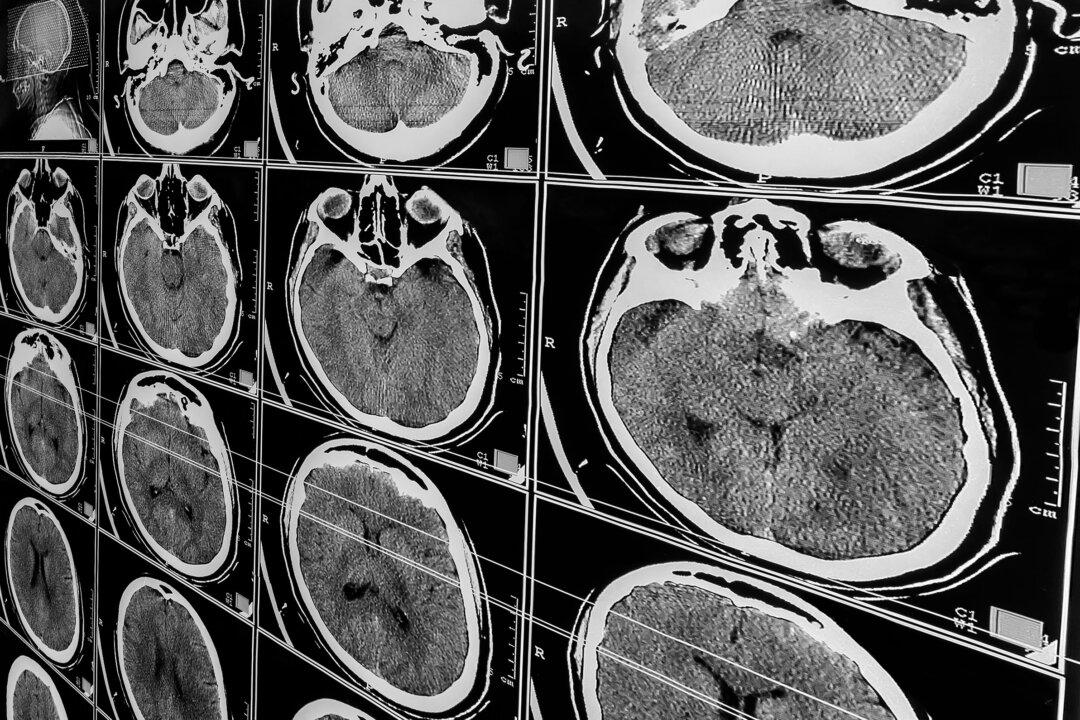
People Near Death From Traumatic Brain Injury May Still Revive: Study
Advanced imaging can detect covert consciousness, offering hope for seemingly hopeless cases, experts say.
6/11/2024
https://www.theepochtimes.com/health/people-near-death-from-traumatic-brain-injury-may-still-revive-study-5658305
When doctors advised pulling the plug on a comatose 22-year-old after a car crash, his mother sought a lifeline from the Brain Rehabilitation and Injury Network (B.R.A.I.N). For weeks, the advocacy group’s founder, Sue Rueb, sat vigil with the unresponsive young man, reading to him for about two weeks.
“All we need, sir,” she said to one of the neurologists, “is time.”
In hospitals nationwide, a final prognosis is delivered 72 hours after a severe traumatic brain injury (TBI)—a mere blink in a race against time that new research warns may be cut short too quickly. New evidence suggests some patients can defy the odds and recover consciousness, even in cases of severe TBI, if only given more time.
Study Calls for a ‘Cautionary Approach’ in Decisions to Remove Life SupportA recent study published in the Journal of Neurotrauma investigated the potential for survival and regaining independence among acute TBI patients who died after the withdrawal of life-sustaining treatment (WLST).
The researchers enrolled over 3,000 TBI patients from 18 trauma centers across the United States between 2014 and 2021. All participants were enrolled within 24 hours of sustaining their brain injuries, and approximately half were followed for one year. Out of these patients, 90 died after having life support removed.
The researchers then matched these 90 cases with similar participants who had not had life-sustaining treatment withdrawn.
While many of those kept on life support eventually died, especially older patients and those with more severe injuries, more than 30 percent of the matched patients were able to recover and achieve some level of independence within six months. At least half of the younger patients with less severe brain injuries regained independence, with some even able to resume their normal lives.
“Our findings support a more cautious approach to making early decisions on withdrawal of life support,” Yelena Bodien from the Department of Neurology’s Center for Neurotechnology and Neurorecovery at Massachusetts General Hospital and a study co-author said in a press release.
TBI Is a ‘Complex’ ConditionA TBI occurs when an external force, such as a blow to the head from a fall, vehicle accident, assault, or another trauma, alters brain function. While TBIs are classified as mild, moderate, or severe, many in the medical community find these categories oversimplified for such a complex condition, Dr. Brent Masel, medical director at the Brain Injury Association of America and not associated with the study, told The Epoch Times.
A significant number of TBI survivors develop long-term issues, he added. The World Health Organization (WHO) defines TBI as a chronic disease process. Potential complications include increased risk of seizures, sleep disorders, neurodegenerative diseases, neuroendocrine problems, psychiatric issues, sexual dysfunction, incontinence, and metabolic dysregulation persisting for months or years.
Life expectancy can also be significantly reduced—by approximately seven years for moderate to severe TBI cases, according to Dr. Masel.
“Outcomes can vary from person to person, and data published by the [U.S. Centers for Disease Control and Prevention] CDC shows that brain injury is a dynamic process with many people improving or getting worse,” Dr. Masel said, noting the condition’s unpredictable nature.
‘Covert Consciousness’According to Dr. Kristen Dams-O'Connor, director of the Traumatic Brain Injury Research Center at Mount Sinai, there are varying levels of consciousness under the umbrella term “coma.”
Coma is a state of unconsciousness where the patient does not react to their surroundings. While comatose, the patient is alive but unconscious, with minimal brain activity and an inability to wake up through physical or auditory stimulation.
When comatose patients require life support, care professionals sometimes have difficult conversations with families about whether the patient would prefer to end life rather than risk living in an undesirable state, Dr. Dams-O'Connor said. She pointed to research conducted by a colleague, Dr. Brian Edlow, who has done work in the area of using advanced neuroimaging to detect something called “covert consciousness.” This is when some patients appear to be unconscious, but they actually have a hidden or covert form of consciousness. They are aware of what’s happening around them, but they cannot express themselves or communicate in the usual ways, like speaking, moving, or making gestures.
The detection of “covert consciousness” through advanced neuroimaging has “fueled a message of hope,” Dr. Dams-O'Connor told The Epoch Times. This sort of imaging can find indicators in the brain that are not detected by clinical evaluations and may have significant prognostic value. Some people who appear to have little hope of recovery may possess covert consciousness, which is associated with improved outcomes.
Risa Nakase-Richardson, a clinical neuropsychologist at the James A. Haley Veterans’ Hospital, has used the TBI Model Systems National Database, which comprises 16 centers across the country, including Mount Sinai, that enroll and follow patients longitudinally from inpatient rehabilitation.
Ms. Nakase-Richardson leads the Polytrauma Rehabilitation Centers, the Veterans Affairs’ equivalent to the civilian model systems of care. Together, they have access to a long-term cohort of individuals, some of whom remain in traumatic disorders of consciousness for months after injury.
Her research found that among patients unable to follow commands at discharge from inpatient rehabilitation, which could be months after injury, 19 percent to 36 percent achieved functional independence five years later, Dr. Dams-O'Connor said. Some TBI patients, advised by doctors to “pull the plug” due to injury severity, lived to become advocates in her research studies. “Their lives may be different, but their lives are very much worth living,” she added.
Given More Time and RecoveredYears later, that young crash victim is walking and talking. To Ms. Rueb, such stories reinforce why referring to “brain-damaged” patients is both inaccurate and demoralizing.
“They’re brain-injured,” she told The Epoch Times, “and the people who have survived it are heroes, in my mind.”
From strokes to gunshot wounds, Ms. Rueb said she had witnessed what seemed to be numerous miracles when families refused to give up on their loved ones too soon after life-altering brain trauma.
No comments:
Post a Comment