This has been obvious from the beginning. Turning that into a medical protocol has never been obvious. Now with the advent of a much deeper understanding through simple scientific research, new protocols are arising.
We are jumping again from BIG focus research to multi focus research and this is welcome.
A flood of real progress is now plausible.
.
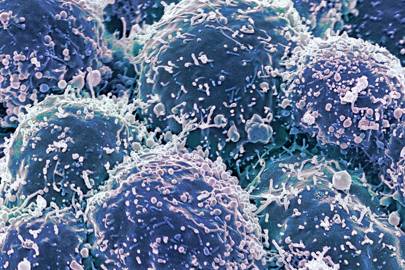
Why your immune system is key in the fight against cancer
Harnessing the power of our immune system will be one of the most important scientific discoveries in history
We are at the dawn of a health revolution. Cancer
physicians agree that immune therapies – the subject of the most recent
Nobel Prize in Physiology or Medicine – is a game-changer, and now sits
alongside surgery, radiation and chemotherapy, as a mainstream option
for the treatment of some types of cancer.
Crucially, neither of the two Nobel Prize winners, Jim Allison and Tasuku Honjo,
directly set out to cure cancer – “that wasn’t it at all,” Allison has
said – they were trying to understand how the immune system works. And
this can’t be emphasised enough: curiosity-driven research won the prize
and brought us new cancer medicines.
Some scientists
do and should focus on understanding cancer or other diseases but we
must also fund science which might seem esoteric – those who are merely
asking what does this or that gene or protein do in the body – because
so many of our greatest discoveries came out of left field. As
cosmologist Martin Rees
once wrote: “A research proposal to make flesh appear transparent
wouldn’t have been funded, and even if it had been, the research surely
wouldn’t have led to the X-ray.”
It was in trying to
understand the details of what two specific receptor proteins did in the
immune system which led Allison and Honjo to stumble upon our immune
system’s brakes. They discovered brakes built into the immune system to
dampen its activity after some time. Brakes act on the immune system to
bring the body back to its normal resting level after a virus, for
example, has been cleared from the body. This led to the idea of using
medicines to block or switch off these brake receptors to unleash a
stronger and longer-lasting immune response to better fight cancer.
Now – with money, people, excitement and
imagination – we should redouble our efforts. The science here is still
relatively new. There are many other receptors, some quite recently
discovered, which also regulate immune cell activity. Each can, in
principle, be blocked to boost (or in some cases dampen) a component of
the immune system. And each can be blocked alone, in combination, or
alongside other therapies.
As well as this, entirely different approaches to immune therapy are also proving successful. One, called CAR T cell therapy,
involves isolating a patient’s immune cells (T cells specifically),
genetically modifying them to include a receptor protein able to target
the person’s cancer, before the cells are then infused back into
patients. This has recently been approved for the treatment of children
with acute lymphoblastic leukaemia, for example. It is not mere hype to
suggest that we are at the dawn of a health revolution.
A
vast global community is continuing this adventure which has opened up
our body’s immune system for what it is; not a part of our anatomy which
can be described with any simple metaphor, like the heart as a pump,
but a multi-layered, dynamic lattice of interlocking genes, proteins and
cells – all of which amounts to one of the most complex and thrilling
frontiers of scientific inquiry in the 21st Century. Unravelling more
details is going to bring us new medicines. Even more so than you might
imagine, because it has recently emerged that the immune system is
intimately connected with an enormous range of diseases, such as heart
problems, neurological disorders, obesity – perhaps nearly all diseases.
Take
one example: Alzheimer’s, the well-known and sadly, relatively common,
cause of dementia. It has long been thought that clumps of amyloid
protein in the brain underlie this disease, but a crucial problem with
is that by the time a patient shows symptoms, the problem has been going
on for some time so that its initial trigger has been notoriously
difficult to identify. One idea to emerge recently is that the amyloid
protein clumps might be part of an anti-bacterial defence in the brain,
and that the real underlying problem might actually be microbes. This is
still controversial but one recent study has suggested that bacteria
which cause gum disease may play a role in Alzheimer’s too. If proven,
this would open up a clear route for immune therapies, or anti-bacterial
medicines, to impact dementia.
Another line of
research has explored the idea of vaccinating against amyloid plaques
directly. Here, an immune response is triggered against amyloid plaques
by vaccination so that a person’s immune system will then be primed to
break down small plaques before they cause a problem. We won’t cure
Alzheimer’s tomorrow, but we have now have found a promising solution:
it’s the immune system, stupid.
Daniel Davis is the author of The Beautiful Cure (Vintage, 2019)
No comments:
Post a Comment