This is all you ever wanted to know about all this. I certainly have encountered cases, but most are partially managed by drugs and pseudo isolation.
most folks have not and today most do not even encounter retardation. It is easiest for victims to remain in the presence of their support group. so public observation is limited.
Again we have made limited progress in terms of therapy.
Schizophrenia: Symptoms, Causes, Treatments, and Natural Approaches
Affecting up to 1 percent of the global population, schizophrenia is a rare but debilitating condition that makes it difficult for one to know what’s real.
SymptomsCausesTypesPhasesRisk FactorsDiagnosisComplicationsTreatmentsMindsetNatural ApproachesPrevention
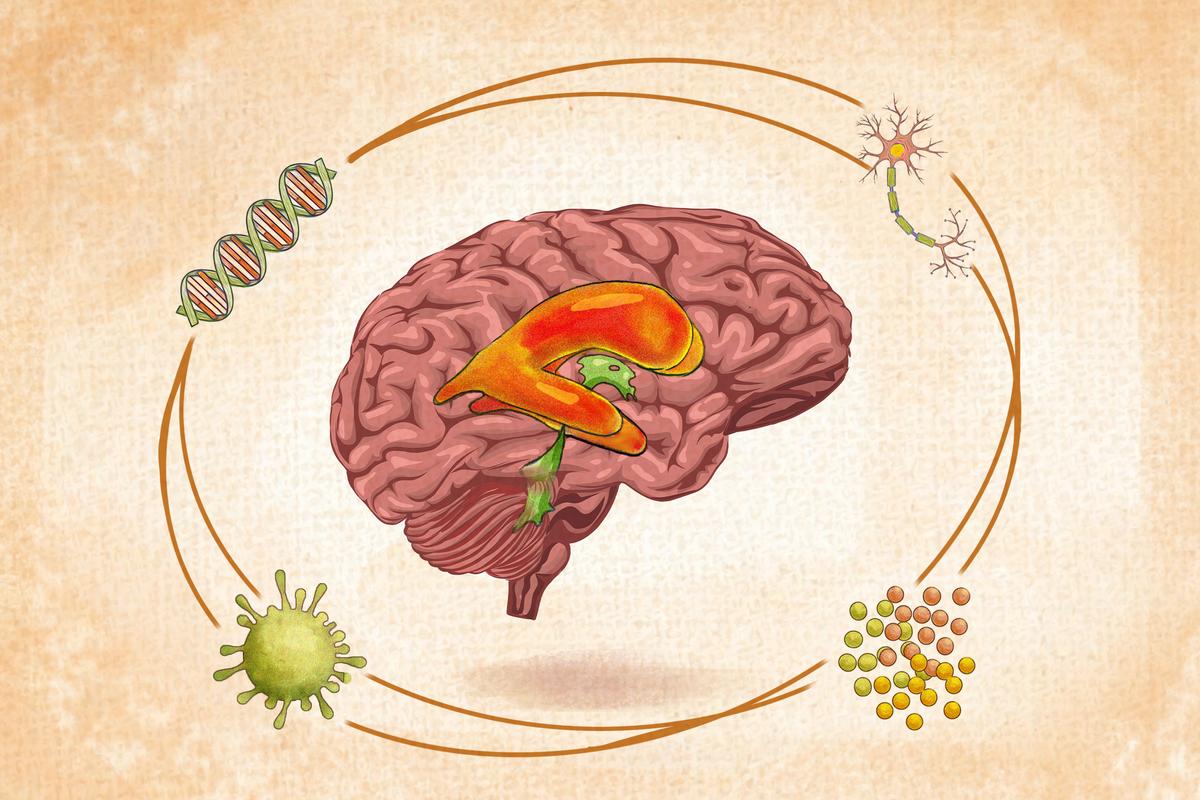
Although the cause of schizophrenia is unknown, a combination of genetic, environmental, and physiological factors plays a role. Pictured are enlarged ventricles, observed in 80 percent of people with schizophrenia. (Illustration by The Epoch Times, Shutterstock)
By Mercura Wang
|
June 16, 2024Updated:
June 17, 2024
https://www.theepochtimes.com/health/schizophrenia-symptoms-causes-treatments-and-natural-approaches-5660614
Schizophrenia is a complex, chronic brain disorder characterized by a loss of contact with reality, hallucinations (auditory), delusions, abnormal thinking, and difficulties in daily functioning.
Estimates of the prevalence of schizophrenia and related psychotic disorders in the United States range from 0.25 to 0.64 percent, with about 24 million (or one in 222) affected in the global population. With accurate diagnosis and appropriate treatment, many people with schizophrenia can lead full lives.
What Are the Symptoms and Early Signs of Schizophrenia?
Many myths exist about schizophrenia. People with this disorder are not intellectually disabled, nor do they have “split personalities.” While some may show aggression during an untreated acute episode, it is rare and unlike the media’s portrayal of serial killers or psychopaths.
Symptoms often first appear when a person is between 15 and 30. Schizophrenia rarely manifests in children under 12. Symptoms can emerge abruptly or progress gradually, possibly without the person’s immediate notice. These vary between individuals and can change over time. Some people have a single psychotic episode, while others experience multiple episodes throughout their lives.
Early SignsAn early phase may occur, during which individuals experience changes in emotion and behavior before the full illness develops. Initial signs might include irritability or tension, difficulty concentrating, trouble sleeping, declining school performance, the belief that others are trying to cause harm, and personality changes (e.g., avoiding social interactions).
There are several types of schizophrenic symptoms, including negative, positive, and cognitive symptoms.
Negative SymptomsInstead of meaning “bad,” negative symptoms refer to aspects of a patient’s personality or experiences that are diminished or absent. They usually appear before positive symptoms. The patient might exhibit the following:Lack of motivation to partake in activities
Neglect of self-care, such as not bathing or eating regularly
Be disinterested in things they used to enjoy
Have inappropriate reactions to everyday life events
Struggle to express emotions
Become angry with strangers without reason and react harmfully to others
Feel detached from their emotions
Have very limited speech
Experience a slowing of movements
Positive SymptomsDespite the term’s implication of something being beneficial, positive symptoms refer to additions or new elements in a patient’s personality or life experience. Common positive symptoms include the following (which, when combined, may be referred to as psychosis):Hallucinations: Changes in perception, such as hearing sounds, seeing things, or feeling sensations that aren’t actually there, are known as hallucinations. These can be auditory, visual, olfactory, gustatory (taste), or tactile, with auditory hallucinations being the most common in schizophrenia.
Delusions: Having persistent, unrealistic thoughts that cause distress, even when others refute them, is delusion, a common symptom of certain mental health conditions. One example is a patient constantly believing in receiving secret messages through the TV.
Confused thoughts, speech, and behavior.
Cognitive SymptomsCognitive symptoms affect a schizophrenic’s thinking processes and are often not noticeable to the person or others. These symptoms can include:Memory loss
Difficulty understanding things well enough to make decisions
Trouble communicating clearly with others
Attention deficit
Suicidal thoughts: Approximately 5 percent to 6 percent of individuals with schizophrenia die by suicide, with around 20 percent attempting it. Many others experience significant suicidal thoughts. Suicide is the leading cause of premature death among people with schizophrenia, contributing to an average reduction in lifespan of 10 years.
What Causes Schizophrenia?
Contrary to popular belief, schizophrenia is not caused by bad parenting, trauma, poverty, or drugs.
Despite its unknown specific causes and mechanisms, schizophrenia has a biological foundation. The neurodevelopmental hypothesis of schizophrenia suggests that a combination of genetic risk factors and environmental factors during early brain development leads to the disorder. These influences, especially during prenatal and early life stages, set the stage for symptoms to appear in early adulthood.
Genetics
Twin and family studies suggest that genetic factors account for roughly 80 percent of the risk of developing schizophrenia. Individuals with a first-degree relative diagnosed with schizophrenia face a 10 percent to 12 percent risk of developing the disorder themselves. If one identical twin is diagnosed with it, the other has about a 45 percent chance of having it. However, many schizophrenia patients don’t seem to have a family history of the illness.
Research has identified at least 130 genes that raise the risk of schizophrenia. Thus, schizophrenia is caused by the combined effects of many different genes, each contributing a small amount to the overall risk. No single gene is responsible for causing the disorder on its own.
Environmental StressorsMany environmental stressors can provoke the onset or return of psychotic symptoms in susceptible individuals. The environmental factors that may contribute to the development of schizophrenia include:Being exposed to viruses or nutritional issues before birth.
Maternal exposure to famine and influenza during the second trimester of pregnancy.
Maternal bacterial infection during pregnancy: A 2019 study found that when mothers experience bacterial infections during pregnancy, it correlates with a higher risk of their children (especially males) developing psychotic disorders such as schizophrenia.
Birth weight under 5.5 pounds (under 2,500 grams).
Rh incompatibility of the mother’s and baby’s blood type in a second pregnancy.
Complications during birth, like oxygen deprivation associated with asphyxia.
Brain Structure and FunctionPatients with schizophrenia exhibit both structural and functional brain abnormalities. Some of the things that can be affected in the brain include:Brain volume: The researchers of a 2014 study involving over 1,200 twins concluded that lower IQ accounts for 25 percent of the total risk variance for schizophrenia, with 4 percent of this variance attributed to smaller brain volume. This suggests that part of the genetic risk for developing schizophrenia may be linked to abnormal early brain development, which leads to cognitive deficits, as indicated by early cognitive changes and smaller intracranial volume in affected individuals.
Anterior hippocampus: A 2019 study discovered that in early-psychosis patients, overactivity in the anterior hippocampus seemed to reduce that part of the brain’s effectiveness when performing tasks.
Auditory cortex: Findings of another 2019 study suggested that one’s susceptibility to auditory hallucinations might be linked to a deviation in how the brain’s auditory cortex is structured from early life, particularly in how it interprets various sound frequencies.
Cortex neurons: A 2017 study suggested that schizophrenia might originate from improperly distributed neural progenitor cells during brain development. This leads to improperly clustered immature neurons in cortical layers and a deficiency of mature neurons in the cortex, which is crucial for memory, thinking, problem-solving, and emotions.
Neurotransmitter levels: In schizophrenia, the levels of neurotransmitters—chemicals that transmit messages between neurons—may vary. Medications that reduce these neurotransmitter levels can alleviate schizophrenia symptoms, indicating their involvement in the disorder’s development.
Ventricles: Brain ventricles produce and store cerebrospinal fluid. Ventricle enlargement is a common hallmark of schizophrenia, with 80 percent of schizophrenics exhibiting it. The reason for this enlargement remains unknown.

Schizophrenia is believed to be caused by a combination of factors, including prenatal conditions, altered structure or function in the brain, and genetics. (Illustration by The Epoch Times, Getty Images, Shutterstock)
What Are the Types of Schizophrenia?
The classification of schizophrenia has evolved over time. As of 2013, the traditional subtypes listed below are no longer officially used in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) developed by the American Psychiatric Association (APA) or the International Classification of Diseases, 11th Revision (ICD-11) developed by the World Health Organization (WHO). Instead, schizophrenia is now thought to exist on a spectrum.
However, to provide a better understanding of the manifestations of the condition, the classic subtypes of schizophrenia are listed below:Paranoid: Paranoid schizophrenia was the most common subtype before being dropped from the DSM-5. Characterized by preoccupation with delusions and auditory hallucinations, it often involves feelings of extreme suspicion, persecution, or grandiosity but with relatively unaffected speech and emotional expression. Paranoia is considered one of the symptoms of schizophrenia.
Hebephrenic: Also known as disorganized schizophrenia, hebephrenic schizophrenia is marked by disorganized speech patterns that are hard for others to understand, inappropriate behavior, flat affect, as well as fragmented delusions and hallucinations. It typically develops when an individual is between 15 and 25 years old.
Residual: Residual schizophrenia applies to people with a history of psychosis, where positive symptoms (e.g., hallucinations or delusions) have significantly diminished, but negative symptoms (e.g., reduced motivation, diminished emotional expression, or slow movement) prevail.
Catatonic: Catatonic schizophrenia is the rarest form of schizophrenia and is marked by disturbances in movement. Individuals with this subtype may exhibit unusual, limited, and sudden movements, switching between being very active and very still. Other symptoms may include echolalia (repeating others’ words) and echopraxia (mimicking others’ movements). Catatonia can occur in a range of other psychiatric disorders and general medical conditions. Around 9.8 percent of adult patients in psychiatric hospitals show signs of catatonia.
Undifferentiated: This subtype is diagnosed when symptoms do not clearly fit into any of the other subtypes but still meet the criteria for schizophrenia.
What Are the Phases of Schizophrenia?
Schizophrenia can progress through many phases, with the duration and patterns of these phases differing from person to person. Typical phases include:Prodromal: Individuals may either show no symptoms or exhibit mild problems such as impaired social skills, anhedonia (loss of pleasure), and general coping deficiencies. These traits can be subtle and recognized only in hindsight.
Advanced prodromal: The aforementioned signs and symptoms of schizophrenia may appear. Less than 40 percent of people in this phase progress to full schizophrenia.
Early psychosis: Symptoms are active and typically at their most severe.
Middle: Symptoms may occur episodically, with identifiable exacerbations and remissions, or they may be continuous. Functional deficits typically worsen in this phase.
Late: The pattern of schizophrenia may become more established but varies significantly.These phases are often simplified into prodrome (when symptoms begin) and active (symptoms become more noticeable or worsen) phases. Although not always formally recognized, residual or recovery phases are sometimes included to indicate diminishing symptoms. In addition, a 2021 cross-sectional study noted high relapse rates, with more than half of the participants relapsing during their lifetimes.
Who Is at Risk of Schizophrenia?
The following factors raise a person’s risk of schizophrenia:Sex: According to a 2003 meta-analysis, the risk of developing schizophrenia was about 1.4 times higher in men than women. However, after the mid-40s, women are more frequently diagnosed with schizophrenia than men.
Age: Schizophrenia typically first appears in young men between 18 and 25 and in young women between 25 and 35.
Family history of schizophrenia.
Birth season: People born in winter or spring are at a significantly higher risk of developing schizophrenia, with those born in these months accounting for up to 10 percent of cases. This birth seasonality link is possibly due to developmental vitamin D deficiency, as there’s less sunlight in winter and spring than in summer and fall.
Upbringing: Growing up in urban settings during childhood raises risk, possibly due to crime victimization and a lack of social cohesion.
Stress: A stressful life event or exposure to dangerous environments increases risk. Immigrants coming into a new country are also more at risk due to the stressful nature of such a move.
Abuse: People who endure childhood sexual abuse are more at risk.
Socioeconomic status: Living in poverty increases a person’s risk.
Cannabis use: Cannabis use, mainly due to cannabis’ psychoactive ingredient THC, can induce temporary psychotic effects and exacerbate preexisting psychotic conditions. Frequent cannabis use, especially daily or near-daily, high-potency cannabis products, and early use before age 16 further increase this risk.
Vitamin C deficiency: A 2022 study showed that low vitamin C levels were common in people with schizophrenia and psychosis, and higher levels had been linked to improvement in difficult-to-treat negative schizophrenic symptoms. The study’s authors concluded that future studies should test whether vitamin C can help with conventional schizophrenia treatment.
Vitamin D deficiency: One 2018 study found that newborns with vitamin D deficiency have a 44 percent higher risk of being diagnosed with schizophrenia in adulthood compared to those with normal vitamin D levels. This suggests that developmental vitamin D deficiency may increase the likelihood of developing the disorder. Developmental vitamin D deficiency refers to insufficient vitamin D during critical periods of development, particularly during pregnancy and early childhood. A 2014 study also discovered that people with schizophrenia who had lower levels of vitamin D exhibited more pronounced negative symptoms and experienced greater cognitive impairments.
Disturbed B-vitamin levels: Several vitamin B deficiencies can cause symptoms of neuropsychiatric disorders. For instance, vitamin B12 deficiency is linked to various neuropsychiatric disorders, and it’s common in chronically ill psychotic patients, even those with adequate nutrition. There have been cases in which vitamin B12 deficiency masquerades as psychotic symptoms in schizophrenia. In addition, a 2018 study found that lower pyridoxine (vitamin B6) levels and higher nicotinamide (vitamin B3) levels are associated with schizophrenia.
Gluten-containing diet: A 2013 study discovered that schizophrenics are 2.13 times more likely to have anti-gliadin IgG antibodies. Gliadin, a protein found in wheat gluten, plays a leading role in gluten-related disorders. This suggests that individuals with schizophrenia may have a higher risk of an adverse immune response to gluten.
How Is Schizophrenia Diagnosed?
Symptoms of schizophrenia must persist for at least six months to confirm a diagnosis.
The primary objective of a schizophrenia diagnosis is to rule out the presence of other medical or psychiatric conditions that may present with similar symptoms, including major depressive or bipolar disorder with psychotic or catatonic features, delusional disorder, schizotypal personality disorder, obsessive-compulsive and body dysmorphic disorder, autism spectrum and communication disorders, and post-traumatic stress disorder (PTSD).
In diagnosing schizophrenia, mental health care professionals such as psychiatrists or psychologists will take a comprehensive medical history and conduct a mental status examination. Information from family members or close contacts is essential and often gathered through interviews. A physical exam, including dermatological exams to uncover signs of substance use or abuse and metabolic syndrome screening, and lab tests may also be performed. Testing for metabolic disorders is vital because of the risks associated with antipsychotic medications.
Although no lab test can diagnose schizophrenia, some are performed to exclude other potential causes. These tests include:Blood tests: Examples include a complete blood count (CBC), an absolute neutrophil count (ANC), and a blood chemistry panel.
Imaging tests: Examples include an electroencephalogram (EEG), a computed tomography (CT) scan, and magnetic resonance imaging (MRI), which is preferred over CT.
Genetic testing.
Drug toxicology screen.To confirm a schizophrenia diagnosis, the clinician refers to either the DSM-5-TR or the ICD-11 criteria, which differ slightly.
DSM-5-TRSchizophrenia is diagnosed when a person experiences two or more of the following symptoms for a significant portion of time within a month or less (if successfully treated):
Delusions
Hallucinations
Disorganized speech
Grossly disorganized or catatonic behavior
Negative symptomsThere must also be a significant functional decline in areas such as work or relationships since the onset of symptoms.
These symptoms must persist for at least six months, with at least one month of active-phase symptoms, which could be shorter if effectively treated. Symptoms can be prodromal (early signs) or residual (lingering symptoms), including negative or less severe active-phase symptoms.
The symptoms should not be due to substance use, medication effects, or other medical conditions. If there’s a developmental disorder present, the diagnosis additionally requires at least one month of prominent delusions or hallucinations.
ICD-11ICD-11 is currently used in the United States as of 2022. According to the criteria, a diagnosis of schizophrenia requires the presence of at least two of the following symptoms for at least one month:Persistent delusions (e.g., grandiosity, persecution, being referenced).
Persistent hallucinations (typically auditory).
Disorganized thinking (e.g., loose associations, irrelevant speech). In severe cases, the person may be speaking in incomprehensible “word salad.”
Experiences of influence, passivity, or control (i.e., the feeling that one’s impulses, actions, or thoughts are not self-generated or that one’s thoughts are being transmitted to others).
Negative symptoms (e.g., flat affect, restricted or loss of speech, disinterest in activities).
Severely disorganized behavior that affects daily life.
Psychomotor disturbances, like catatonic restlessness.At least one of these must be among the first four symptoms listed.
The ICD-11 goes into more detail about determining a diagnosis, but these are the main criteria.
What Are the Possible Complications of Schizophrenia?
The possible complications of schizophrenia include:Severe cognitive impairments, like memory loss and attention deficit
Social withdrawal and isolation
Suicide
Physical health issues, like cardiovascular, metabolic, and infectious diseases
Inability to attend school or keep a job
Alcohol or drug abuse
Other co-occurring mental disorders, such as obsessive-compulsive disorder (OCD)
Aggressive or violent behavior
What Are the Treatments for Schizophrenia?
Although a cure doesn’t exist for schizophrenia, its symptoms can be managed in some cases. The earlier and more intensive the treatment, the better the outcome.
A patient-centered plan that combines nonpharmacological and pharmacological approaches is essential in treating schizophrenia. Usually, more than one treatment method is used. The treatment methods are as follows.
1. MedicationDifferent types of medications are used in treating schizophrenia.
Antipsychotics, also called neuroleptics, are the main medications used for schizophrenia, as they are the most effective in controlling symptoms such as delusions and paranoia. They control these symptoms by altering brain chemistry. However, antipsychotics can cause side effects, including dizziness, restlessness, sedation, slowed movements, tremors, weight gain, diabetes, and high cholesterol. There are two types of antipsychotics:First-generation antipsychotics (FGAs): Long-term use of FGAs, including haloperidol, fluphenazine, and chlorpromazine, may increase the risk of tardive dyskinesia, a movement disorder, as well as other extrapyramidal symptoms, which are severe side effects affecting the extrapyramidal system (part of the brain and nervous system) involved in coordinating movement. Extrapyramidal symptoms are common in some patients using antipsychotics and may be associated with impaired cognitive performance.
Second-generation antipsychotics (SGAs): SGAs, or atypical antipsychotics, particularly olanzapine and clozapine, pose a higher risk of metabolic syndrome.There are also FGA and SGA long-acting injectable antipsychotics to help address treatment nonadherence. When administered at intervals ranging from weeks to months, these medications gradually release their active ingredients into the bloodstream, ensuring a consistent therapeutic effect.
Maintenance antipsychotic drug regimens for schizophrenia aim to reduce the frequency and severity of relapses, maximize treatment effectiveness for persistent symptoms, and improve treatment adherence.
Individuals with schizophrenia may also use antidepressants, mood stabilizers, and sedatives.
2. Brain Stimulation TherapiesPatients with schizophrenia may also undergo brain stimulation therapies, such as electroconvulsive therapy (ECT) and transcranial magnetic stimulation (TMS).
ECT is a medical procedure mainly used for severe depression or bipolar disorder. It involves a short electrical pulse to the brain under anesthesia and is done by a specialized medical team. Some doctors also recommend using ECT to treat schizophrenia. A 2018 review concluded that ECT was not only useful as an adjunctive therapy in treatment-resistant schizophrenia but could also be effective in treating patients with schizophrenia in different situations. Research also indicates that ECT is a safe treatment option for schizophrenia.
TMS uses magnetic pulses to stimulate nerve cells in the brain. Rapidly changing magnetic pulses can alter the firing pattern of neurons in specific brain circuits, which can help modify dysfunctional brain patterns associated with schizophrenia. A 2015 review found that repetitive TMS showed promise in alleviating both positive and negative symptoms of schizophrenia, with a notable impact on reducing auditory hallucinations.
3. Estrogen TherapyResearch indicates that estrogen may offer protective benefits for women susceptible to schizophrenia. A 2024 review suggested that estrogen supplementation could be considered as an adjunctive treatment for people with schizophrenia, particularly those with poor response to antipsychotics, as this approach might improve symptom control, offer cognitive enhancement, and delay illness onset.
4. Talk TherapiesAlso known as psychosocial treatments, talk therapies help patients examine and understand their thoughts and behaviors. There are several types of talk therapies, including:Cognitive behavioral therapy (CBT): CBT teaches individuals to modify beliefs or behaviors that lead to negative emotions through two main components: cognitive, which changes thinking, and behavioral, which changes reactions. This short-term, problem-focused therapy aims to provide coping skills for managing difficult situations and is typically administered for one hour a week over 12 to 16 weeks.
Art therapy: Art therapy can help people express and understand their feelings, learn new ways of relating to others, and accept their emotions. It is particularly useful for depressive symptoms such as social withdrawal, as it often involves group sessions that combine communication with creativity.
Family intervention: This involves working with mental health professionals to help patients and their families manage relationships.
Cognitive remediation: This treatment aims to restore a patient’s cognitive functions. It involves practicing tasks to enhance attention, memory, reasoning, and other cognitive functions.
5. Rehab and Self-HelpRehabilitation and support programs, such as on-the-job coaching, psychosocial skill training, and vocational rehabilitation programs, teach skills needed for living in a community rather than an institution.
Self-help and management for schizophrenia involves focusing on exercise, diet, relationships, and daily routines. It also includes taking medication, recognizing triggers and signs of an episode, maintaining recovery, and knowing where to seek help in a crisis.
How Does Mindset Affect Schizophrenia?7
Mindset can play a significant role in how individuals experience and cope with schizophrenia.
Mindsets can influence a patient’s coping strategies. A positive mindset might lead to the adoption of healthy coping mechanisms, such as seeking social support and engaging in therapy. On the other hand, a negative mindset might result in avoidance behaviors or substance abuse, which may exacerbate the symptoms.
A resilient mindset can help individuals with schizophrenia better manage stressors in their lives by developing coping skills and cultivating a sense of optimism.
Maintaining a positive mindset can motivate people to stick to their treatment plans, potentially reducing symptoms. It can also contribute to a patient’s positive beliefs about himself or herself (self-esteem) and one’s abilities, thus leading to greater resilience, motivation, and a sense of control over one’s life.
What Are the Natural Approaches to Schizophrenia?
The effectiveness of some of the natural treatments for schizophrenia presented below needs further research for confirmation, so please consult your doctor before using any of these treatments.
1. Medicinal HerbsIndian snakeroot (Rauwolfia serpentina): Indian snakeroot is an evergreen shrub native to southeast Asia. It has been primarily used for treating hypertension and as an antipsychotic compound. Reserpine, extracted from Indian snakeroot, has been used in conventional medicine as an antihypertensive and antipsychotic medication. A 2024 study on 60 male patients found Indian snakeroot potentially beneficial in treating positive symptoms of schizophrenia as a homeopathic remedy. However, it is not yet recommended over more effective treatments until more robust clinical trials can provide evidence of safety and efficacy. Because it lowers blood pressure, people with hypotension should not take it.
Ashwagandha (Withania somnifera): Also known as Indian ginseng, ashwagandha has long been used in Ayurvedic medicine with anti-inflammatory and immunomodulating properties. A 2018 randomized controlled trial on 66 patients found that after using the herb’s extract as an adjunctive treatment for 12 weeks, schizophrenia patients experienced substantial reductions in negative and overall symptoms compared to the group that didn’t receive the extract.
Ginkgo (Ginkgo biloba): Also known as a “brain herb,” ginkgo has been widely used for memory issues. A 2010 meta-analysis of six studies found that adding ginkgo to antipsychotic medication significantly improved both total and negative symptoms in patients with chronic schizophrenia. As per a 2013 meta-analysis of three studies, ginkgo can also reduce positive symptoms in schizophrenia patients. A 2005 study found that ginkgo extract might enhance the effectiveness of antipsychotics in schizophrenics, especially in alleviating positive symptoms.
Yokukansan: Also known as yi-gan san, yokukansan is a traditional Chinese medicine used widely in Eastern Asian countries. It contains seven herbs, including Angelica, Atractylodes, Bupleurum, Poria, Glycyrrhiza, Cnidium, and Uncaria. In a 2009 clinical trial, schizophrenia patients used yokukansan for four weeks, and their positive and negative symptoms significantly improved. Also, no drug-induced extrapyramidal side effects were observed. The researchers suggested that yokukansan could potentially be used for treatment-resistant schizophrenia.
2. Supplements
Vitamin C: A 2022 study indicated that schizophrenia patients often have lower vitamin C levels than healthy individuals. Another older clinical trial from 2005 suggested that taking vitamin C along with SGA medications can reduce oxidative stress and improve schizophrenia symptoms.
Vitamin D: Vitamin D is crucial for brain functions such as learning and memory, producing brain chemicals, protecting brain cells, and transmitting signals. A 2021 study in BMC Psychiatry found that vitamin D supplementation combined with antipsychotic treatment can improve attention span and alleviate positive and negative symptoms in schizophrenia patients previously with vitamin D deficiency. A 2018 study showed that 12 months of vitamin D supplementation in nonhospitalized, vitamin D-deficient schizophrenic patients was linked to reduced depressive symptoms and lower rates of anxiety.
B vitamins: Folate (vitamin B9) and vitamin B12 supplementation can improve the negative symptoms of schizophrenia, although the treatment response is affected by genetic variations in folate absorption. A 2017 clinical trial concluded that high-dose pyridoxamine (a form of vitamin B6) as an additional treatment was partially effective for a subgroup of schizophrenia patients experiencing increased carbonyl stress, a marker of an abnormal metabolic state.
Omega-3 fatty acids: Omega-3 supplementation appears to be particularly beneficial for young adults and adolescents in the early stages of schizophrenia who initially have low levels of omega-3 fatty acids by improving negative symptoms and global functions. Some evidence also suggests that omega-3 fatty acids have the potential to either prevent schizophrenia or at least alleviate its course and symptoms.
3. DietsGluten-free: Antigliadin antibodies (AGA) are markers of gluten (a protein in wheat and some other grains) sensitivity and are higher in people with schizophrenia. A small 2019 pilot feasibility study found that schizophrenia patients who followed a gluten-free diet showed improvements in their gastrointestinal and negative symptoms, but no improvement was observed in positive or cognitive symptoms.
Ketogenic: The keto diet is a low-carbohydrate, high-fat diet. Its goal is to shift the body’s metabolism from primarily using glucose (sugar) as its energy source to using ketones, produced from fats. It has shown promise in normalizing schizophrenia-like behaviors in both pharmacological and genetic mouse models. This diet can also improve psychiatric symptoms, metabolic dysfunctions, and body composition in patients with schizophrenia by restoring brain energy metabolism.
4. Eye Movement Desensitization and Reprocessing (EMDR)EMDR is a therapy approach designed to ease the distress linked with traumatic memories, and it has been used to treat PTSD. A 2020 systematic review of six studies found that EMDR was linked to reduced paranoid thinking, auditory hallucinations, delusional symptoms, and negative symptoms in individuals with psychosis.
Overall, it seems to be a safe and feasible intervention. In a 2021 case study, after receiving one single EMDR session, a patient with chemically resistant schizophrenia experienced a complete remission of the disorder and disorganization/dissociative syndrome within eight weeks. This remission was also sustained, allowing the interruption of antipsychotic treatment without relapse for 18 months.
5. Alternative TherapiesEcotherapy: Ecotherapy is a therapeutic approach that utilizes outdoor activities in natural environments as part of the treatment. These activities can range from conservation work and gardening to walking or cycling in nature.
Yoga therapy: In a 2007 study, after four months of practicing, patients in the yoga therapy group exhibited notably lower levels of psychopathology than those in the physical exercise group. When combined with antipsychotic medications, yoga improves treatment outcomes for both positive and negative symptoms compared to medications alone. A 2012 systematic review of randomized trials also indicated that yoga may improve both positive and negative symptoms, in addition to health-related quality of life in patients with schizophrenia. In addition, antipsychotic medications can lead to obesity in schizophrenia patients, but yoga therapy has been found to mitigate this weight gain.
Acupuncture: A 2023 meta-analysis of 38 randomized controlled trials found that acupuncture, used along with conventional antipsychotics, improved symptoms of schizophrenia and reduced the incidence of adverse reactions. An older 2009 meta-analysis of 13 Chinese studies also found that combining acupuncture with drug therapy led to a notable improvement in auditory hallucinations, positive symptoms, and response rates as opposed to using antipsychotics alone.
Meditation: In one 2018 study, five severely affected schizophrenia patients, each with a medical history spanning over two decades, underwent an eight-month mindfulness meditation program and experienced decreased abnormal brain activities and hallucinations or delusions, as well as improved anxiety and psychotic symptoms. It took three weeks before the symptoms began to alleviate. Additionally, a 2024 systematic review of 22 studies found that mindfulness-based interventions offered potential benefits for schizophrenia patients, including decreased negative symptoms and lowered hospitalization rates.
How Can I Prevent Schizophrenia?
Preventing schizophrenia entirely isn’t feasible as its exact cause remains unknown. Still, you can lower your risk by making the right lifestyle choices and following a treatment plan to prevent symptoms from resurfacing or worsening. Specific strategies include:Avoiding drugs and alcohol: Substance use can complicate the treatment of schizophrenia.
Getting enough sleep: Adequate sleep is crucial to avoid exacerbating symptoms.
Managing stress: Stress can worsen schizophrenia symptoms.
Eating healthily and exercising regularly: A nutritious diet and regular exercise can ensure adequate levels of vital nutrients, mitigate symptoms, promote good sleep, and manage stress.
Adhering to a treatment plan, if you have one: As stopping medication can lead to symptom recurrence, any changes or discontinuation of drugs should be managed solely by the prescribing health care provider.
Avoiding triggers to psychotic episodes.
Understanding warning signals: Establish a strategy to manage symptoms promptly and seek appropriate assistance.
Using support services: A range of comprehensive support services, including housing and supportive employment opportunities, can help you reduce stress.
No comments:
Post a Comment