Unexpected and promising and likely to be sooner than later. so many antibiotic protocols have aged out quickly and really faster than we can make them up.
now it would be nice if this can be applied to all those other antibiotics as well. no.t likely, but we can dream.
in spite of problems we have saved millions of lives so far.
New Antibiotic Targets Only Harmful Microbes
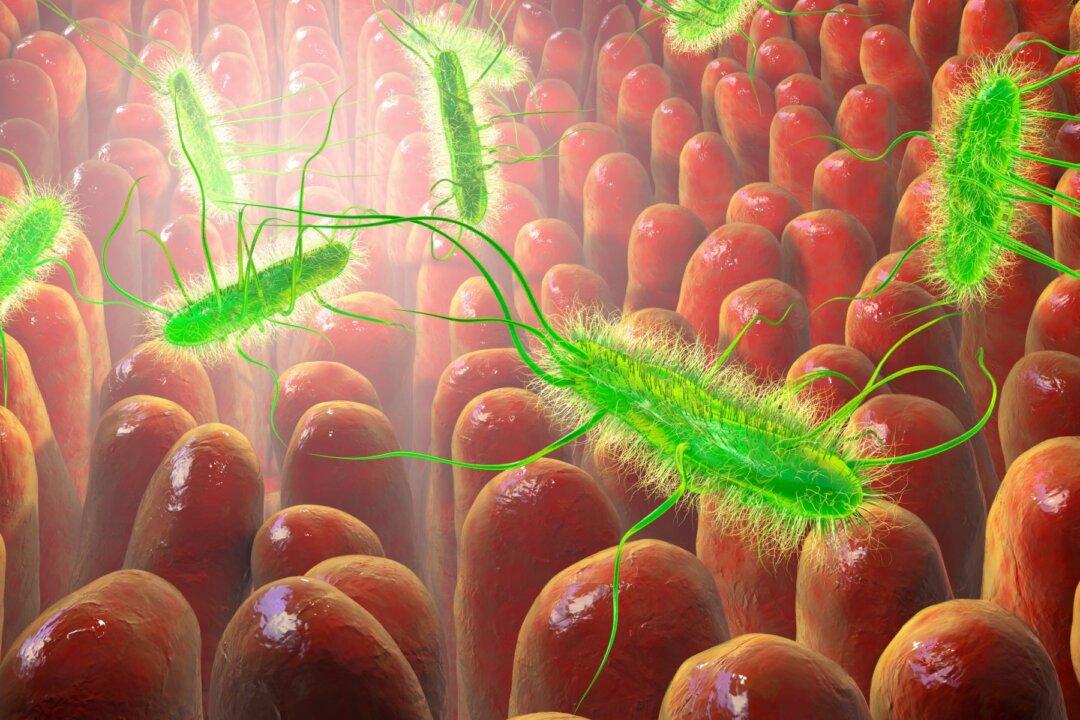
Antibiotics non-selectively destroy both harmful and beneficial gut bacteria, but there is now potential to preserve the good.
By Huey Freeman
Researchers believe they have created a new kind of compound, an antibiotic that kills only the worst microbes, without producing dangerous side effects.
Scientists at the University of Illinois took on the challenge of developing an antibiotic that kills gram-negative bacteria which are often resistant to antibiotics, without destroying microbes necessary for good health. If bacteria do not develop resistance to this drug, it could be a significant breakthrough in treating infections for years to come.
Chemistry professor Paul Hergenrother, co-leader of the study, said people are waking up to the realization that life-saving antibiotics also have serious side effects.
“They’re killing our good bacteria as they treat the infection,” Mr. Hergenrother said in a press release. “We wanted to start thinking about the next generation of antibiotics that could be developed to kill the pathogenic bacteria and not the beneficial ones.”
The study focused on killing infectious gram-negative bacteria, which are harder to kill because they have a double layer of protection. Drugs used in hospital settings that destroy harmful gram-negative bacteria also fight against beneficial bacteria, said Kristen Muñoz, lead author of the study.
“Most clinically approved antibiotics only kill gram-positive bacteria or kill both gram-positive and gram-negative bacteria,” Ms. Muñoz said in the press release.
Ms. Muñoz said colistin, an antibiotic prescribed to fight only gram-negative bacteria, has been known to cause diarrhea, as well as colitis, a potentially fatal condition. Colistin has also caused harm to the liver and kidney, so it is “typically utilized only as an antibiotic of last resort,” the scientists wrote in their study.
Blazing a New TrailThe research team became interested in finding a better antibiotic because there has not been a U.S. Food and Drug Administration (FDA)-approved antibiotic in more than 50 years targeting gram-negative bacteria, which are incredibly problematic and difficult to treat, said Ms. Muñoz, in an interview with The Epoch Times.
Ms. Muñoz said virtually all antibiotics used in clinics cause an imbalance in the gastrointestinal tract, “because they do not discriminate between the good bugs and the bad bugs.” The goal of this research was to find an antibacterial agent with “the potential for selectivity for gram-negatives over gram-positives, and had further selectivity for pathogens over commensals.” Commensal bacteria protect the immune system from invasion by pathogens.
The new drug, lolamicin, has been found to be effective in mice in cases of acute pneumonia and septicemia, a bloodstream infection. Sepsis, a complication of septicemia, causes about 270,000 deaths out of the 1.7 million adult cases each year in the United States, according to the Centers for Disease Control and Prevention.
“I think the biggest takeaway from this research is the double-selective component of lolamicin,” Ms. Muñoz said. “Here we were able to develop a drug that not only targets problematic pathogens, but because it is selective for these pathogens only, we can spare the good bacteria and preserve the integrity of the microbiome. This initial study of lolamicin opens up the door for implementing this double-selective strategy for the future development of microbiome-sparing antibiotics. We hope that the impact of lolamicin can bring about a new generation of targeted antibiotics.”
Exciting DiscoveryMs. Muñoz said that during the testing phase of many more bacterial strains, in vivo of mice, the researchers were excited to see that their hypothesis for developing narrow-spectrum antibiotics was promising. The microbiome of mice is a good tool for modeling human infections because the gut microbiomes of mice and humans are similar, she explained. Antibiotics that cause an imbalance of microbes in mice have similar effects on humans.
“It was very exciting when I first made this compound and discovered it was active against critical gram-negative pathogens,” she said. “Perhaps more importantly though, we are most interested in the impact lolamicin could have on the future development of microbiome-sparing antibiotics.”
Lolamicin was also found to prevent secondary infections with Clostridioides difficile, a serious bacterial infection commonly associated with hospitals. It was found to actively fight against more than 130 bacterial strains in cell cultures, all of which were resistant to multiple drugs.
In order to formulate the compound lolamicin as a marketable antibiotic, the manufacturers will have to consider many factors, including solubility, pH measurement, and optimal crystalline form, Ms. Muñoz said. Other considerations will include dosage and form of medication, such as liquid, tablet, or injection.
“We are still a bit away before we get to formulating this compound as an antibiotic,” she said. “There is a long road ahead for lolamicin before it receives FDA approval. Unfortunately, it can take more than 20 years from the time of antibiotic discovery to when an antibiotic gets clinically approved. In the meantime, we will continue to study lolamicin. We want to keep testing the drug against more bacterial strains and perform more detailed toxicology studies.”
No comments:
Post a Comment