what we still do not have is a good biological pathway that gives us so called bad cholesterol and statins are not surviving the test of time.
what i do know is that independent of all this ,is that we all suffer from low level scurvy which can be countered by a daily heaping teaspoon of ascorbic acid or vitimin C. As per Linus Pauling who turmed a bad prognosis at age 48 into a full life through 92. my own prognosis was also equally bad after my own heart attack at age 57. the last looksee five years ago showed zero new inflamation and all old scaring just that. And i do expect to see 100 with a healthy circulatory system.
otherwise, i would like to have far better answers than any of this which assumes the association is significant when it may well not be. Far too often meta stats throw up indications that are simply that and certainly no proof of causation..
'Silent' killer in cholesterol more firmly linked to heart disease
June 13, 2023
Common problem: One in five people have the genetic potential for elevated Lp(a) levels
https://newatlas.com/medical/silent-killer-cholesterol-lpa-heart-disease/?
A genetic ‘bad’ cholesterol protein has been flagged as a hidden problem in coronary heart disease (CHD), with current medication that treats low-density lipoproteins (LDL) having little effect on this particular variant.
In an observational study of 607 adults aged 60 and over, across 16 years, levels of lipoprotein(a) – known as Lp(a) – were both higher and more prevalent in those who had experienced a recurrent CHD event. While this doesn’t go as far as proving direct causation, it does highlight a link and shines a light on the need for Lp(a)-targeted therapies.
“This finding adds to growing evidence of a relationship between increased Lp(a) and the risk of recurrent CHD,” said lead author Leon Simons, associate professor at the School of Clinical Medicine, at the University of New South Wales Sydney. “It is well-established that people who have already experienced CHD are at very high risk of another event.
“Our new results indicate that new therapeutics in development that aim to reduce elevated Lp(a) might help prevent recurrent disease,” added Simons, who has been working on resolving the mysteries of this macromolecular complex for decades.
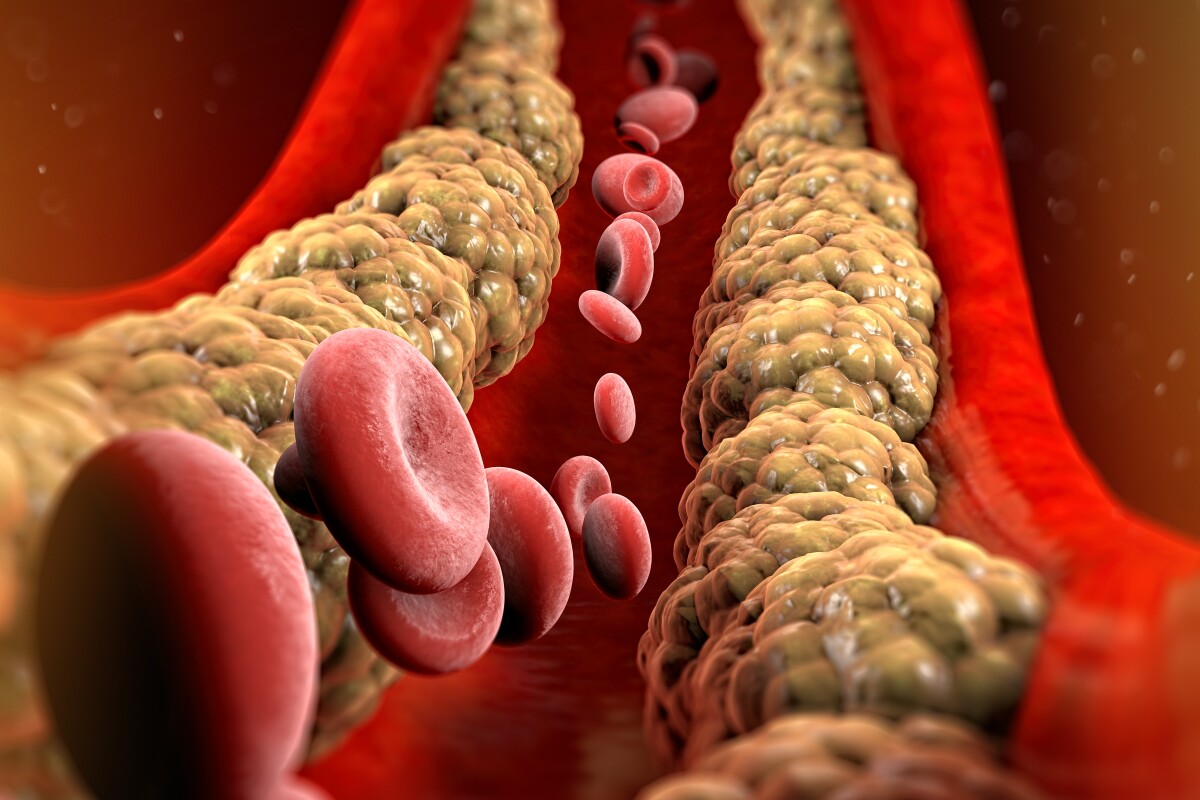
Lipoproteins, which also includes high-density lipoprotein (HDL), are the mechanisms by which cholesterol is moved around the bloodstream. HDL is generally considered the good, because it takes its piggybacked cholesterol to the liver, where it can be removed from the body.
LDLs, on the other hand, are responsible for cholesterol build-ups on artery walls. Lp(a), also found in human plasma, is assembled from LDL and a large hydrophilic glycoprotein called apolipoprotein(a). And it has structural elements from the lipoprotein and blood clotting systems linked to premature CHD and stroke. Earlier research has highlighted its role in heart attack and stroke.
Lp(a) levels are 75-95% heritable, and an estimated one in five people are born with the genetic coding for it. But while most adults in the US will be screened for cholesterol, a common blood test won't check for Lp(a) levels; fewer than 1% will be screened for this variant to the LPA gene. (On the plus side, because it's genetic, levels remain consistent throughout life so frequent testing isn't required.)
It’s also particularly insidious, as high levels of Lp(a) are unlikely to present with any noticeable physical symptoms. For some, the first evidence of their elevated risk is a heart attack.
This study also revealed that adults with prior CHD, elevated Lp(a) levels of more than 355mg/L presented a 53% risk of recurrent heart attacks, when compared to those in the study with the lowest levels (below 50mg/L) during the 16-year period.
"Elevated Lp(a) is an important predictor of recurrent CHD in older people,” said Simons. “Upper reference Lp(a) levels of 500 mg/L or 300 mg/L both appear to be appropriate for identifying those at higher risk who may benefit from more intensive risk reduction interventions.”
Lp(a) levels may not yet be the target of medical intervention, but risk can be mitigated diet and exercise, which is recommended for anyone with all ‘bad’ cholesterol readings. Researchers hope more understanding into the role Lp(a) plays in cardiovascular disease will lead to medical intervention that can better target it.
“While current medications, such as statins, are often prescribed to lower ‘bad cholesterol’ in patients at higher risk of cardiovascular disease, these do not have any major or proven impact on elevated Lp(a),” Simons said. “But there is hope for the future – as some novel therapeutics that are designed to lower the levels of Lp(a) are currently in the advanced stages of clinical development.”
No comments:
Post a Comment