What a kiss to your health. Again, what i am most concerned with is the establishment of end points. just when does all this stop? We are all prepped to handle biological insults and to usually shake them off.
I strengthen mine by maintaining vitimin C saturatiion.
what this is realloy like is a robust cold sore that does not go away or simply migrates to otger parts of the skin. Not good.
Atypical Small–Fiber Neuropathy Occurrence After COVID-19 Vaccination, Possibly Underdiagnosed
Unexplored COVID-19 Vaccines Adverse Events (Part 4)
Apr 25 2023
https://www.theepochtimes.com/health/atypical-small-fiber-neuropathy-occurrence-after-covid-19-vaccination-possibly-underdiagnosed_5163697.html
In this series, we evaluate some of the lesser-known yet common adverse events that are appearing in the research literature as well as in doctors’ clinics and, more importantly, how to deal with them and reduce the risks.
Three days post-vaccine, former Pussycat Dolls member Jessica Sutta woke up to “the most excruciating muscle spasms” that were unlike anything she had ever experienced, she said.
“It felt like I’d broken my rib,” Sutta said.
As an athlete and a professional dancer, she had broken her rib before on tour, “so I know pain very well,” she said in an exclusive interview on “American Thought Leaders.”
Sutta tried her typical therapies—seeing the chiropractor, doing acupuncture, getting massaged, and resting—but the muscle spasms and pain persisted, worsening into burning and stabbing pain in her sides.
She admitted herself to the hospital and was run through several laboratory tests, but her results showed that everything was normal.
At the same time, Sutta started to hear about reports from other people who had experienced neurological problems following the COVID-19 vaccination, but it was too hard for her to make the connection. She told her husband, who showed her a video related to vaccine adverse events, to turn it off, saying, “‘No way. This is just a muscle spasm. It’s going to go away.'”
However, her continued attempts with different remedies resulted in new debilitating symptoms.
Sutta was finally referred to a neurologist by her general practitioner.
“[My general practitioner] finally let me see him, and the first thing he said was, ‘When did you get the vaccine?'” she said. “He goes, ‘I think you had an adverse reaction.’
“That was the first time that I acknowledged it was actually happening to me.”
The pain Sutta experienced was small fiber neuropathy. She described it as feeling like she was being subjected to fire.
“It would come in contractions, it would come in waves, and it was so debilitating, and I just didn’t know what to do,” she said.
Unfortunately for Sutta, her neuropathy remains today.
According to the Vaccine Adverse Event Reporting System (VAERS), more than 1,600 cases of peripheral neuropathy have been reported after the administration of COVID-19 vaccines, and about 150 cases of small fiber neuropathy have been reported.
One woman, Caroline Bollinger, developed chest pain and tingling, numbness, and burning pain in her upper limbs 10 days after receiving a COVID-19 mRNA vaccine.
While her symptoms have since dissipated, she told The Epoch Times that they still flare up once in a while.
Less Classic Presentation in Vaccinated People
Since the advent of the COVID-19 vaccines, neurologists Dr. Diane Counce and Dr. Suzanne Gazda have been seeing many novel neurological manifestations among their patients.
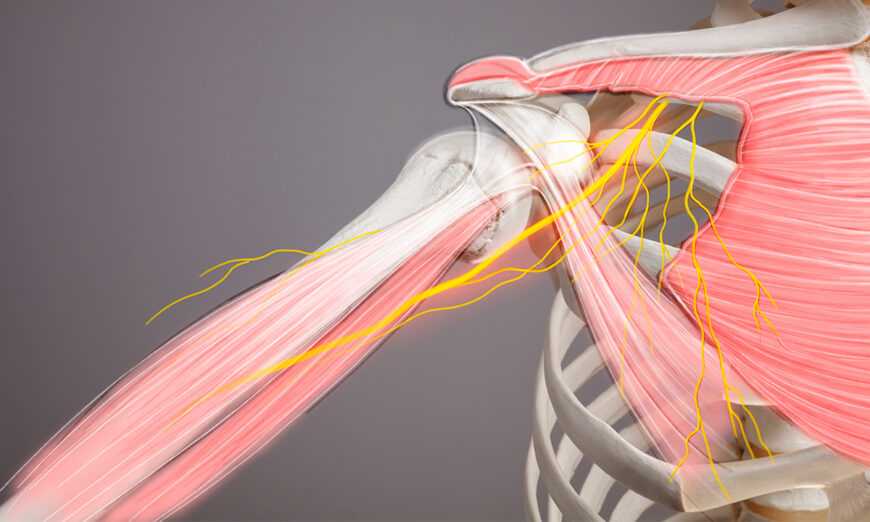
Counce said a common neurological complication she sees is peripheral neuropathy. These are diseases that affect neurons outside of both the brain and spinal cord—including nerves in the internal organs, limbs, and skin.
Among them, small fiber neuropathy is the most common.
Small fiber neurons detect pain and temperature, hence why small fiber neuropathy is often associated with tingling, numbness, pins-and-needles, and burning sensations.
Some small fiber neurons are autonomic neurons, so diseases in small fibers can lead to impairments in sweating, blood pressure, heart rate, digestion, excretion, vision, and many other functions.Functionals of peripheral nerves.
Source: Cassellini, Carolina & Vinik, Aaron (2007), ‘Clinical manifestations and current treatment options for diabetic neuropathies’, Endocrine Practice, vol. 3, no. 5, pp. 550-566. (The Epoch Times)
Heat intolerance and impaired or excessive sweating are common manifestations of small fiber neuropathy and can occur in the absence of pain.
Since symptoms and severity are highly variable, Dr. Svetlana Blitshteyn, an associate professor of neurology at the University of Buffalo said the disease could be significantly underdiagnosed.
In the United States, small fiber neuropathy is usually associated with diabetes. Diabetic neuropathy is known as the classic small-fiber neuropathic presentation. This is where numbness, tingling, pins-and-needles, or pain initially sprout in the fingers and toes, gradually moving up the limbs in a stocking and glove formation as the disease worsens. Due to its prevalence, the diabetic neuropathic pattern is the most recognized, neurologist Dr. Matthew Bain told The Epoch Times.
There are also less common presentations of small fiber neuropathy. These include all peripheral neuropathies that don’t follow a stocking and glove pattern; the arms may be affected before the hands, or the head, chest, and torso areas may be the first places affected. The neuropathy can also be migratory, meaning that the numbness, tingling, and pain can change places from time to time, making it even harder to diagnose the disease.
Counce, who has treated about 300 patients who developed symptoms postvaccine, told The Epoch Times that while acute and long-COVID patients tend to follow the classic diabetic-like patterning, the small fiber neuropathies linked to the COVID-19 vaccine can be atypical.
“I had one [vaccinated] patient whose entire shoulder was burning, but her hand felt okay,” she said. “She ended up being a small fiber neuropathy patient, and then I’d have some [vaccinated] people and their face feel like it’s burning or the middle of their back feels like it’s burning.”
Similar presentations have been reported by Sutta, who initially experienced painful muscle spasms in her core that then developed into burning small fiber neuropathies that radiated across her lower ribs and spine.
Counce also had a patient whose neuropathic regions would change every session.
Autoimmunity Implications
Gazda argues that these neuropathies are likely to be caused by autoimmunity, which occurs when the body attacks its own tissues. Coincidentally, less common presentations of small fiber neuropathies are also strongly linked with autoimmune diseases.
Autoimmunity from COVID-19 vaccines may occur if local blood vessels produce spike protein and become attacked by immune cells and antibodies, as has been shown in autopsy presentations by German pathologist Arne Burkhardt.
The spike proteins share many features with human proteins. Research by immunologist Dr. Aristo Vojdani shows that antibodies made against the spike protein could also attack at least 28 different human tissues.
Board-certified internist and founder and medical director of the Center for Balanced Health Dr. Keith Berkowitz said he would observe abnormal patterns where peripheral neuropathies occur with fatigue, mental fog, and tinnitus.
Small Fiber Neuropathy and COVID-19 Vaccines: Research
Several studies have linked COVID-19 vaccines to small fiber neuropathy.
A 2022 National Institutes of Health-funded study that hasn’t yet been peer-reviewed detected signs of small fiber neuropathy in half of the COVID-vaccinated people.
The study evaluated 23 people who developed neurological symptoms within a month of receiving their primary COVID-19 vaccines. None of them had a prior history of neurological diseases, most had no history of autoimmune diseases, and all developed symptoms within three weeks of vaccinations.
Another case study, published in January in the European Neurology Journal, concluded that an mRNA COVID-19 vaccine was causal to the small fiber neuropathy manifestations in a 39-year-old male.
The patient developed tingling, numbness, and pain in his left shoulder within 10 days of vaccination. These symptoms then progressed to his two arms, hands, and feet.
Within three weeks, he developed muscle twitching and numbness in his feet and hands, the areas burning if touched. Punch biopsies taken from the patient’s left foot and leg showed abnormally thin, small fibers which returned to normal density after treatment with antibody infusions.
While fewer than 200 cases of small fiber neuropathies occurring after COVID-19 vaccination were reported to VAERS, symptoms that may be associated with small fiber neuropathies (pdf), such as itchiness, which has nearly 40,000 reports, and abnormal sensations, loss of sensation, and excessive sweating, have more than 20,000 reports.
Impaired sweating and heat regulation are major indicators of small fiber neuropathy. Studies have put the Quantitative Sudomotor Axon Reflex Test (QSART) forward as a more accurate diagnostic test for small fiber neuropathy than the common skin biopsy. QSART tests for sweat activity.
Since skin biopsies are usually taken in the feet and legs, this may not be a suitable test for atypical presentations, given that the pain may also occur in the face, stomach, ribs, and shoulders.
However, the QSART machine is very expensive and unavailable in most clinics. Blitshteyn noted that patients would need to go to large university hospitals or major clinics to do these tests, which is why small fiber neuropathies—especially atypical presentations—are easily misdiagnosed.
Limited Treatments
While there are several anti-epileptic and antidepressant drugs used as first-line treatments for addressing small-fiber neuropathic pain, the results haven’t been too promising, with low overall effectiveness.
Blitshteyn said that, compared to symptom relief, it’s more important to find drugs that can address the cause of neuropathic pain.
She believes that autoimmunity and inflammation underlie long-COVID and postvaccine small fiber neuropathies, but there are few anti-inflammatory and immune-modulating therapies approved for such purposes.
According to Blitshteyn, some studies have mentioned steroids as a treatment option for small fiber neuropathy postvaccine. Intravenous infusion with antibodies, also known as IVIG, as well as plasmapheresis, have also been suggested to address inflammation and autoimmunity.
Steroids are approved for small fiber neuropathy, and while Blitshteyn has seen them lead to clinical improvements in some patients, they aren’t viable in the long term.
Both Gazda and Counce have used IVIG to treat their patients experiencing neuropathies linked to an autoimmune response. However, this treatment is expensive, and since it isn’t FDA-approved for small fiber neuropathies, insurance-based patients may not get reimbursement.
IVIG’s effectiveness is also subject to debate, with some studies finding negligible differences between IVIG and a placebo (saline solutions).
Some studies have reported success in using low-dose naltrexone and alpha-lipoic acid to treat small fiber neuropathy. Critical care expert Dr. Pierre Kory found low-dose naltrexone to be quite effective in his patients, but studies have been limited.
Apart from therapies for neuropathic sensory discomfort, small-fiber neuropathy is also associated with autonomic dysfunction, which can be a lot harder to treat. Dysautonomia, a form of autonomic disorder, is incurable.
Novel Presentations Complicate Diagnosis and Treatment
Another problem Gazda and Berkowitz noted was that many of the neurological adverse events postvaccine don’t occur as a single symptom. That’s because many different biochemical and metabolic pathways are affected.
Patients may present with fatigue, brain fog, cognitive decline, tinnitus, movement disorders, autonomic dysfunction, or symptoms that may be unrelated to neurological complications.
Specialty doctors may be overwhelmed by the many symptoms that coexist and affect each other.
“If you’re a neurologist, you don’t necessarily know how to treat it if it is going to be an autoimmune problem or a vascular immune problem,” neurologist Dr. Robert Lowry told The Epoch Times.
Another problem with novel postvaccine presentations is that doctors may be hesitant to make a diagnosis, Berkowitz said. Patients may be tested multiple times before doctors prescribe any treatment.
Gazda said it’s important for doctors to be open to considering the role vaccines may have played and that they research how vaccine-induced spike protein pathways may affect the body. This approach will give some patients a better chance to recover.
Blitshteyn, who was the first doctor to notice the connection between dysautonomia and the human papillomavirus (HPV) vaccine, said that while postvaccine small fiber neuropathy exists, she sees more patients who are suffering from the same condition because of long COVID. She said that, therefore, such findings don’t necessarily discourage people from getting vaccinated.
Other doctors such as critical care pulmonologist Dr. Joseph Varon, who co-authored prophylactic and early treatment protocols for COVID-19, said if patients were treated and or cleared for COVID-19 early, there was a very low chance of developing sequelae, or aftereffects of disease.
Next: More than the underdiagnosed cases of postvaccine small fiber neuropathy, some doctors are more concerned about the slew of novel movement disorders they’re seeing in their patients.
No comments:
Post a Comment