First off, i do not think that anyone trys too hard with the elderly and most cases today are just that.
Otherwise, rare young victims are in fact cured of one type or the other, so it is not a wash. It is still a tough trip. again, it is rare enough.
this should have been solved by now though and we certainly have to wonder why not?
Is Leukemia Truly Incurable and Fatal?
Surprising treatment breakthroughs in recent years
FEATUREDCANCER
Jan 14 2023
There have been surprising breakthroughs in the treatment of leukemia in recent years. (Shutterstock)
Leukemia is a term that scares many people. It is commonly known as blood cancer and is a malignant disease involving the blood system. But is leukemia truly incurable and fatal? How has leukemia’s treatment method and its effectiveness progressed in recent years?
The Epoch Times interviewed Michael Andreeff, a professor of medicine in the Department of Leukemia, Division of Cancer Medicine at the University of Texas MD Anderson Cancer Center in Houston, Texas, regarding the above questions. This article is written and organized based on the content of the interview.
Classification and Diagnosis Methods of Leukemia
Leukemia can be divided into two groups, chronic and acute, and it can be further divided into lymphocytic leukemia and myelogenous leukemia according to its cell of origin.
Therefore, in general, there are four main types of leukemia: chronic lymphocytic leukemia (CLL), acute lymphocytic leukemia (ALL), chronic myelogenous leukemia (CML), and acute myelogenous leukemia (AML).
The causes and gene mutations of these four types of leukemia are all different—they are not related to one another and have great differences, and their treatment and prognosis are also completely different.
The symptoms of leukemia are not distinct. Patients may feel tired or bleed for no apparent reason. It may not be discovered until a doctor checks the blood counts and finds that they are not normal.
A blood count measures the number of three types of cells in the blood: red blood cells (which contain hemoglobin) that carry oxygen, white blood cells that protect against infection, and platelets that stop bleeding.
White blood cells and red blood cells in the blood. (Shutterstock)
Leukemia patients may have at least three or four abnormalities in their blood count.
For example, their hemoglobin levels may be low, which can cause the patients to feel tired because there is not enough oxygen in the blood.
Their white blood cell count may also be too low or too high. Low white blood cell counts indicate that patients do not have enough cells to fight infection and are prone to fevers, which require prompt treatment and can be fatal. On the other hand, an influx of abnormal leukemia cells produced by the bone marrow and released into the blood can cause a high white blood cell count.
The platelet count may also be low. Some patients have very low platelet levels, leading to spontaneous bleeding without trauma.
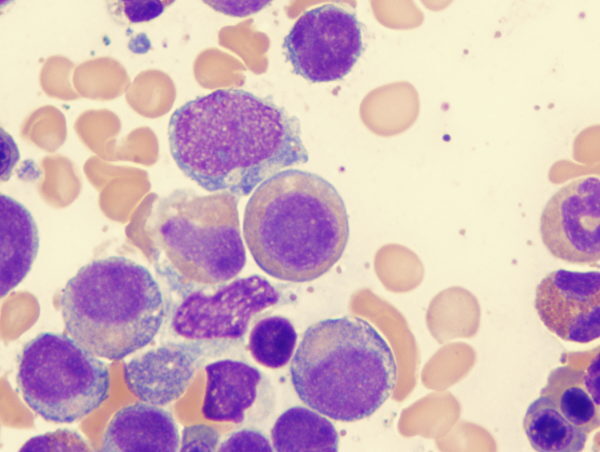
Blood count results alone are not enough to diagnose leukemia; a bone marrow test is also needed. Bone marrow tests can only determine the type of leukemia, but special tests (such as ones that look for mutated genes and abnormal chromosomes, immunophenotyping, etcetera) can also be performed. These special tests are conducted because there are many immunotherapies and gene-targeted therapies for leukemia.
Chemotherapy Can Cause Leukemia
Because we know so little about its causes, there is currently no feasible or complete way to prevent it, but we do know some of the risk factors that may lead to leukemia.
These days, most cancer patients are treated with chemotherapy. A study found that patients who received chemotherapy for other cancers had a higher chance of developing leukemia in the future, and this is related to Clonal Hematopoiesis of Indeterminate Significance, or CHIP cells.
As people age, a small number of cells in the blood begin to turn abnormal and develop genetic mutations, but these cells are not abnormal enough to cause leukemia or other cancers. These are called CHIP cells.
In such context, chemotherapy treatments for breast, ovarian, lung, and other cancers may transform CHIP cells into a preleukemic state, which may develop into leukemia in the future.
For instance, myelodysplastic syndrome (MDS) is a precursor to acute myelogenous leukemia (AML), and MDS is often seen in patients receiving chemotherapy for solid tumors.
Myelodysplastic syndromes are a group of disorders caused by abnormal production of blood cells in the bone marrow. (Shutterstock)
As it seems patients who received chemotherapy for other cancers also have an increased risk of developing leukemia in the future, the current research trend is to replace chemotherapy with other methods, such as immunotherapy.
Exposure to benzene has also been linked to acute myelogenous leukemia. Found in solvents used to wash and degrease machine parts, as well as in some glues used to treat such parts, benzene has been associated with a risk of leukemia.
Radiation can also cause leukemia. Eight years after the atomic bombing of Hiroshima, the number of confirmed cases of chronic myelogenous leukemia in the Hiroshima area reached its peak. It can be inferred that radiation-induced leukemia may take eight years or even longer to develop.
X-rays and radiation used for medical diagnosis can also be a problem. Hence, while CT scans are useful, they should only be done when necessary.
Additionally, certain lawn fertilizers have been linked to the development of chronic lymphocytic leukemia or lymphoma.
Most Cases of Chronic Myelogenous Leukemia Can Be Completely Cured
Among the four types of leukemia mentioned above, chronic myelogenous leukemia (CML) has made the most progress and has the best treatment effectiveness.
Chromosomal abnormalities have long been noted in the leukemia cells of most CML patients. Such abnormalities were first discovered in Philadelphia, Pennsylvania, hence the name the “Philadelphia chromosome.”
It was not until 1982 that the gene mutation caused by the Philadelphia chromosome was discovered, and the mutation was confirmed to be a single-gene mutation. The first-generation drug targeting the abnormal gene was introduced in 2001 after extensive scientific research and clinical trials, and it instantly changed the three-and-a-half-year average life expectancy of CML patients at the time.
Since then, the survival rate of CML patients has greatly increased, and today, the treatment success rate of the targeted therapy is almost 100 percent, which is simply a dream result.
Gene mutations caused by the Philadelphia chromosome also exist in the leukemia cells of some ALL patients. The treatment success rate of such patients after receiving the targeted therapy is also very high.
High Survival Rate for Chronic Lymphocytic Leukemia, Many Patients Remain Disease-Free in Remission
Another type of leukemia with a long survival period is chronic lymphocytic leukemia (CLL), which is mainly seen in the elderly, with the average age of patients being 70 years old. It is more common in Western countries and less common in Asian countries.
Symptoms of CLL include swollen lymph nodes in the neck, armpit, or groin, and an enlarged spleen. In addition, patients may have very high white blood cell counts. Doctors generally do not start treatment as long as the patient is in good condition.
However, the approach is changing, and more doctors are considering early intervention for CLL. This is because the longer the waiting period, the more chromosomal and other molecular abnormalities become present in the patient’s leukemia cells.
Currently, CLL can be treated with methods like chemotherapy and gene-targeted therapy. Chemotherapy has significantly improved the survival rate of patients, while gene-targeted therapy is effective for almost all CLL patients.
It takes a longer observation period to determine whether a patient is completely cured, as CLL is inherently a slow-evolving chronic disease.
Doctors tend to be conservative and will not claim that a patient is completely cured. However, CLL patients are expected to have a long life expectancy. Most CLL patients can stay in a leukemia-free remission state, and many of them will recover. Relapsed patients now have access to alternative medicines, which were not available 10 years ago.
The Deadliest Leukemia Can Be Treated With Arsenic, With a Cure Rate of 90 Percent
There is an extremely critical and dangerous subtype of acute myelogenous leukemia (AML) called acute promyelocytic leukemia (APL).
In addition to abnormal white blood cells in the body, APL patients also have coagulation disorders. If left untreated, the patient usually bleeds to death within a few weeks, or even overnight.
As a result, the early mortality rate of APL patients was up to 30 percent, and the overall survival rate was only 30 percent. This type of leukemia is also the most difficult to treat.
Worse, these patients do not experience early warning symptoms, and they often say, “I’ve never been sick.” However, the leukemia had been developing in their body for years; it simply did not cause symptoms until later on.
Surprisingly, the drugs developed (pdf) to save the lives of APL patients are a form of the vitamin, all-trans retinoic acid (ATRA), and the highly toxic substance arsenic trioxide (commonly known as arsenic).
After clinical verification, all-trans retinoic acid and arsenic have become the standard drugs for treating APL all over the world, and they have indeed achieved the effect of stopping bleeding and saving patients’ lives.
The cure rate of APL has reached 80 to 90 percent worldwide, and the effectiveness of the disease’s treatment can only be described as miraculous.
APL only accounts for 15 percent of the total number of AML patients, and great progress has been made in the treatment of the remaining AML patients.
Different AML patients have mainly relied on two kinds of drug treatment for more than 50 years, and the cure rate is only about 20 to 25 percent. However, 10 new drugs have been approved by the FDA in the past three years, and the response rate of elderly AML patients to treatment has reached nearly 90 percent. Many patients are expected to be cured, though the exact results are still being observed.
CAR-T Cell Therapy for Acute Lymphocytic Leukemia Is a Huge Progress
The treatment of acute lymphocytic leukemia (ALL) still requires many sessions of chemotherapy, but it can be tolerated by children’s bodies and the cure rate is close to 90 percent, which is amazing.
Treatment outcomes in adults with ALL are significantly worse than in children, but high remission rates can still be achieved. Patients in remission usually remain in good health, and there is no trace of leukemia on microscopic or molecular testing.
In addition to chemotherapy, immunotherapy is an essential treatment method for ALL. One of the commonly used immune drugs is a monoclonal antibody that can be mass-produced. The antibody recognizes and binds to protein antigens on the cell surface, ultimately destroying the leukemia cells. Immunotherapy has significantly reduced the relapse and mortality rate of ALL patients.
Natural killer cells kill cancer cells. (Shutterstock)
Another emerging cancer treatment involves collecting a patient’s normal white blood cells, genetically modifying them, and then returning them to the patient. These cells, called CAR-T cells, kill leukemia cells.
This treatment method for ALL has been approved by the FDA. It has been clinically proven that CAR-T cell therapy is effective in about half of ALL patients who do not respond to any other treatment, which is a huge improvement.
Except for Some Types, the Cure Rate of Leukemia Is Increasing Year by Year
Generally speaking, the cure rate of leukemia patients is increasing year by year, and a significant change in the survival curve can be seen every five years; some types of leukemia even reach a 90 percent cure rate. However, it is undeniable that the cure rate for some types of leukemia remains extremely low.
For example, a type of leukemia with a mutation in the P53 gene barely responds to any current treatments.
Even with drugs available, there is one big problem in leukemia treatment, and that is high drug prices. For example, a targeted drug for CML costs $100,000 per year in the United States.
It takes an average of 20 years and a huge amount of capital for a drug to go from development to animal testing, to three phases of clinical trials, and eventually to FDA approval. Most people cannot afford such expensive drugs. Some patients have no choice but to travel to other countries in search of cheap generic drugs.
However, it is possible to access free medicine in the United States.
During the clinical trial phase of a drug (which usually lasts several years), patients participating in the trial are given free medication, including other standard drugs used in combination.
Drug companies sometimes also provide free access to many drugs that have been approved by the FDA. While many patients can still obtain free drugs even if their insurance company does not cover their costs, this requires the cooperation of a professional team to fight for the patients’ access.
Is It Worth Participating in a Clinical Trial for the Treatment of Leukemia?
Many people think that participating in clinical trials and using new drugs that have not been approved by the FDA is tantamount to treating themselves as guinea pigs, but this is not the case.
“Patients will not die from the use of new drugs, only from cancer,” Andreeff said.
A lot of preliminary work is required before any new drug can enter large-scale clinical trials. A team of experts consisting of chemists, pharmaceutical chemists, and doctors works in the laboratory for years prior to a drug receiving approval. Every new clinical trial needs to be approved by the FDA before it can start, and there are many safeguards under the supervision of the FDA.
Furthermore, doctors recommend experimental new drugs only when they think patients will benefit from them.
Even if patients do not experience substantial therapeutic responses after participating in clinical trials, or the experimental new drug is not approved by the FDA in the end, participating in such clinical trials may prolong patients’ lives.
Statistics have shown that patients participating in clinical trials live longer than those receiving standard treatment elsewhere.
In specialized cancer centers with abundant information and resources, some cancer specialists have access to information about new drugs, and they already know the effectiveness of those drugs long before the FDA approves them. Even after new drugs are approved by the FDA, it may take a while before oncologists can start using them.
As a doctor who works at a large specialized cancer center, Andreeff believes that it is best for patients to start treatment at one of these cancer centers, or at least consult the specialists there for a second opinion, so as not to miss out on treatment options that may be right for them.

No comments:
Post a Comment