I suspect that I had a close encounter with this monster at the very beginning when it was first distributed by CCP operatives. It drove a sinus infection that lingered for six months before dissapating. No one could then identify it yet alone correctly test for it.
My defense was that I am vitimin C saturated by consuming about 8000 mgs per day and also some natural quinine, but not at the beginning. The quinine may actually have finished it off.
understand every cell in our body need vitimin C in order to destroy viruses it comes in contact with.
this is all conjecture though and now that most folks have taken the jab, they are more vulnerable to the infection. again do get on vitimin C. It also stops circulatory disease..
Jab Injuries, 50% Long COVID Cases Have This Type of Symptom—2 Ways to Reverse It
0:0014:26
1
https://www.theepochtimes.com/jab-long-covid-half-of-symptoms_4683758.html?
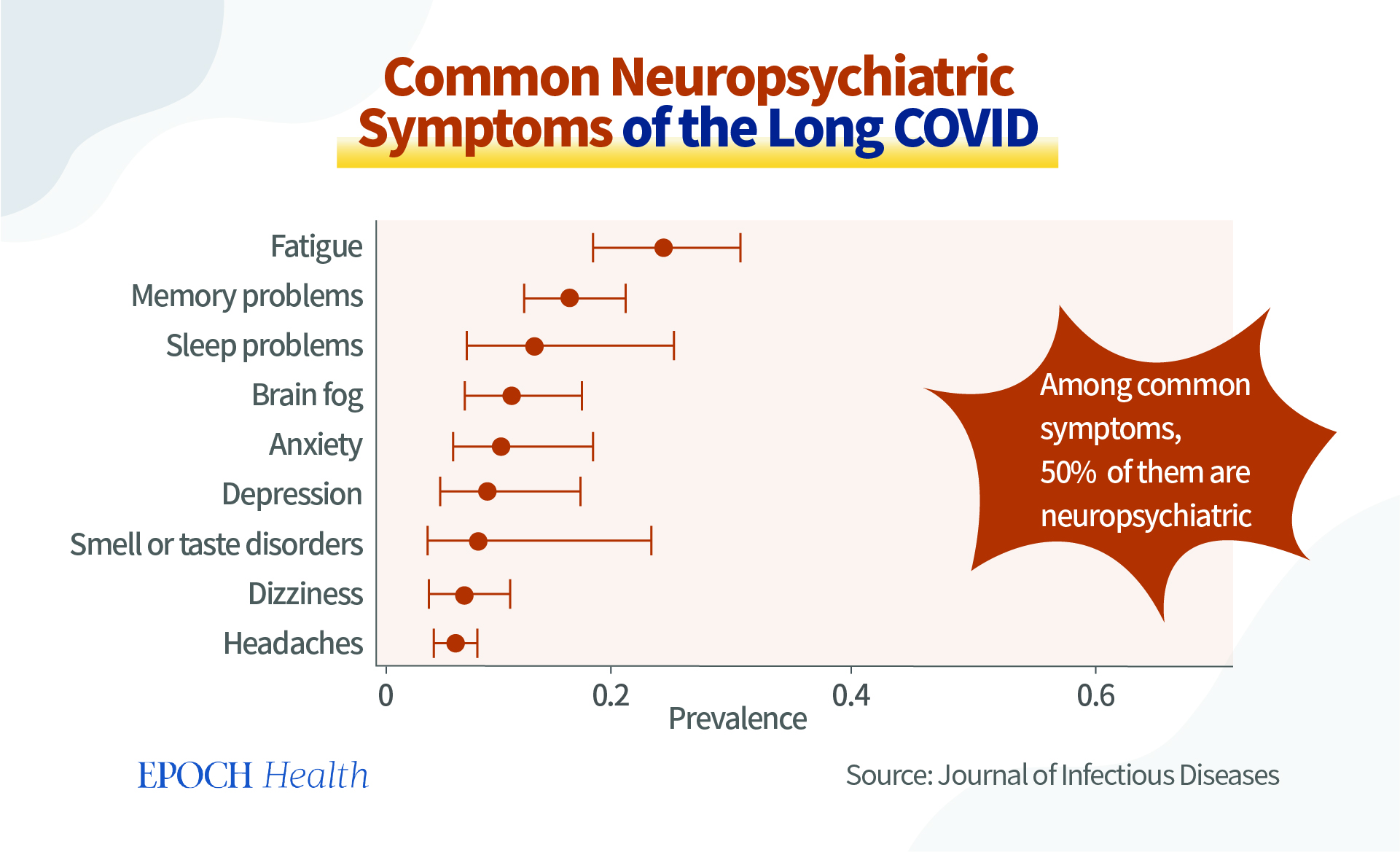
Many people experience “long COVID” symptoms after an acute attack of COVID-19 infection. Half of them are neuropsychiatric and show obvious symptoms. How do COVID-19 infections damage the brain and nerves?
There are two ways to improve these damages.
Half of All Long COVID Cases Have Psychiatric and Neurological Symptoms
According to a study published in the Journal of Infectious Diseases in 2022, among the top 18 symptoms of long COVID, 50 percent of them are neuropsychiatric ones, including memory problems, sleep problems, brain fog, anxiety, depression, smell or taste disorders, dizziness, and headaches.
An article in the journal Science suggests that vaccination may also cause rare symptoms similar to those of long COVID.
These symptoms can have a significant impact on people’s daily work and life.
To find effective solutions, we first need to understand how the SARS-CoV-2 virus damages one’s neuropsychiatric system.
The SARS-CoV-2 Virus Can Cross the ‘Blood-brain Barrier’ and Attack the Brain
First, the SARS-CoV-2 virus can enter the brain.
In healthy people, the brain is firmly protected by the blood-brain barrier, so harmful substances and immune cells generally cannot break into the brain under healthy conditions.
However, in an article published in The Lancet Neurology, a neuropathological analysis of the brains of 43 patients who passed away due to COVID-19 found that most of them had inflammation and immune activation in the brain. Eighty-six percent of the patients had astrocyte proliferation in all areas of the brain that were examined. These cells usually accumulate at the sites of neuronal damage, and an abnormal presence of immune cells was found in the brains of 76 percent of the patients.
These immune triggered pathological changes are expected. However, what is more surprising is that SARS-CoV-2 virus proteins were directly detectable in the different brain regions of 53 percent of these patients, including the neuronal center controlling respiratory and cardiac functions in the lower part of brainstem (connective part between cerebrum and spinal cord).
Furthermore, experiments with primates have also shown that the SARS-CoV-2 virus can directly damage nerve cells, causing them to degenerate and even die.
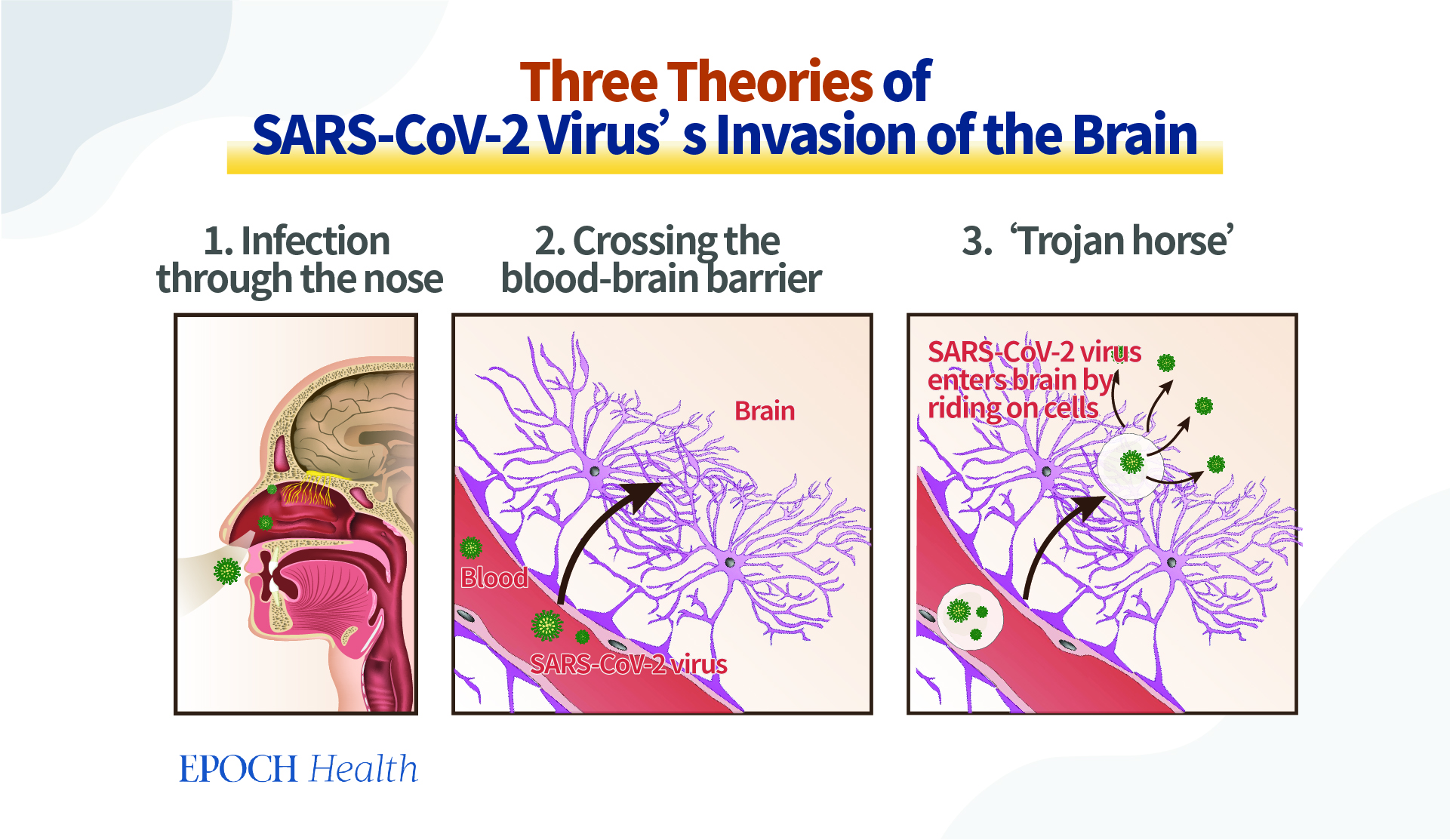
How does the SARS-CoV-2 virus cross the blood-brain barrier and infect the brain and nerve cells?
Currently, there are three theories that are widely discussed and even accepted by the academic community:
After being inhaled into the nasal cavity, the virus binds to ACE2 receptors in the olfactory nerve terminals and thus enters the central nervous system in a way of reverse axonal transportation.
After the virus enters the endothelial cells of the blood vessels, it could be released by these cells, enter into other cell layers, and then finally break through the blood-brain barrier.
The virus enters into the immune cells in the peripheral blood and “rides” on them to cross the blood-brain barrier like soldiers in a Trojan horse.
What will the virus do to the neurons then?
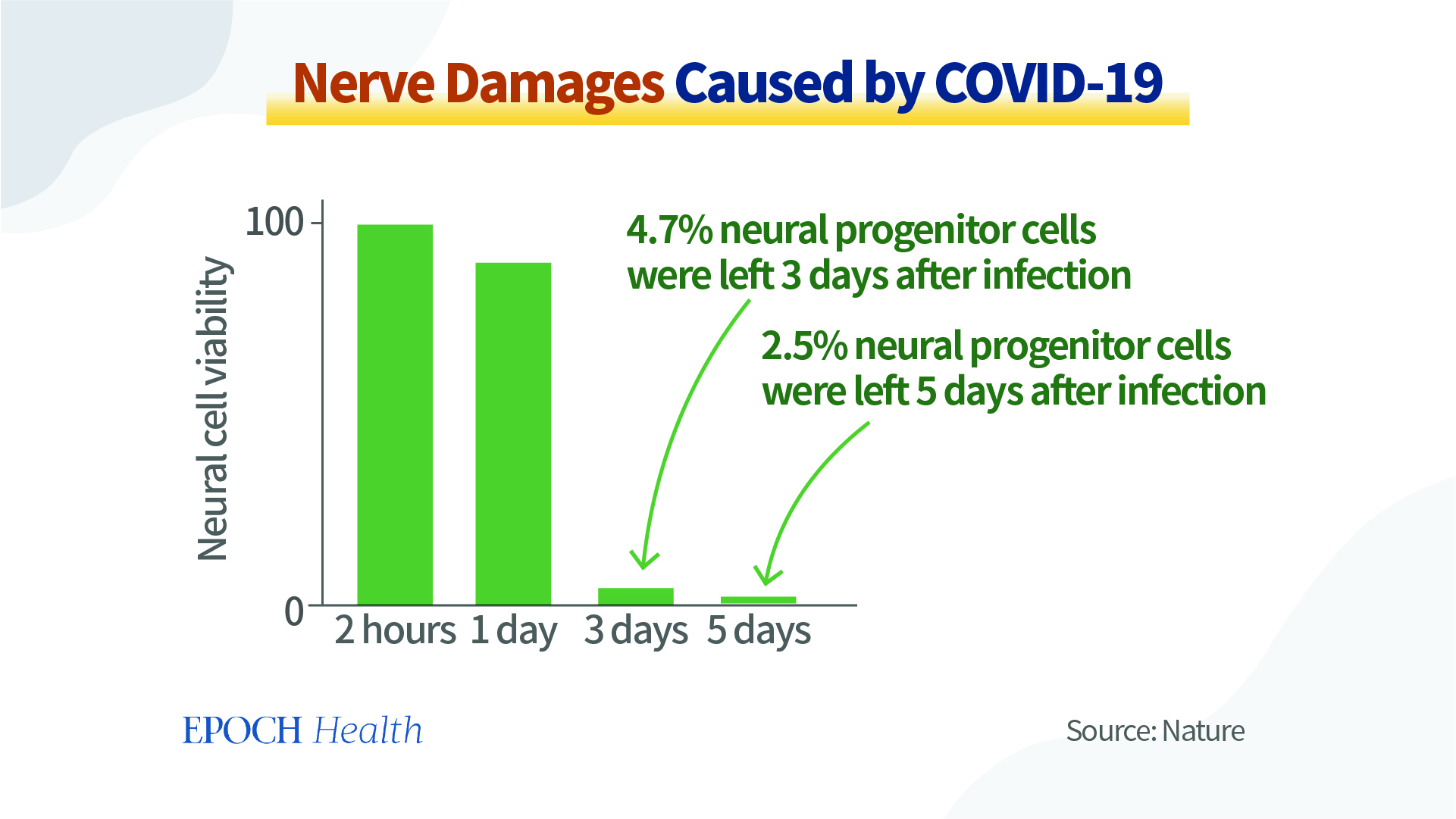
Experiment: 3 Days after COVID Infection, Only 5 Percent of Neural Progenitor Cells Were Left
A study published in the journal Cell Research found that the SARS-CoV-2 virus not only replicates in neuronal cells, but also causes the apoptosis (cell death) of neural progenitor cells. Only less than 5 percent of neural progenitor cells survived for 3 days after the COVID infection, and the percentage dropped to less than 2.5 percent after five days.
Why does the SARS-CoV-2 virus cause such severe damages to neural cells? The mechanism of the SARS-CoV-2 virus’s damage to nerves is summarized in a review published in the journal Nature.
In addition to directly affecting the brain and nerve cells, inducing cell death, the SARS-CoV-2 virus can attack blood vessels, causing ischemia (restricting blood flow) and hypoxia (lack of oxygen) in the brain; the antibodies to the virus can also bind to the normal brain components, resulting in autoimmune attacks on the brain nerves.
Furthermore, we have summarized before that the COVID disease can cause cytokine storms resulting in inflammation in the nervous system; and they can damage the mitochondria of nerve cells and lipid metabolism disorder. We explained these in detail in the article Why Long COVID and Vaccine Injuries Look so Similar: Expert Explains.”
SARS-CoV-2 Virus Inhibits ‘Autophagy,’ Affects Brain’s Self-Renewal
In addition to these reasons, a recent article published in the journal Developmental Cell found that the SARS-CoV-2 virus can inhibit the cells’ autophagic process.
The concept of autophagy was first introduced in 1974 by Belgian cell and biochemist Christian de Duve, who was awarded the Nobel Prize in Physiology or Medicine.
Literally, autophagy means “eating oneself.” It is an important physiological mechanism for cells to digest and reuse waste products and to renew themselves.
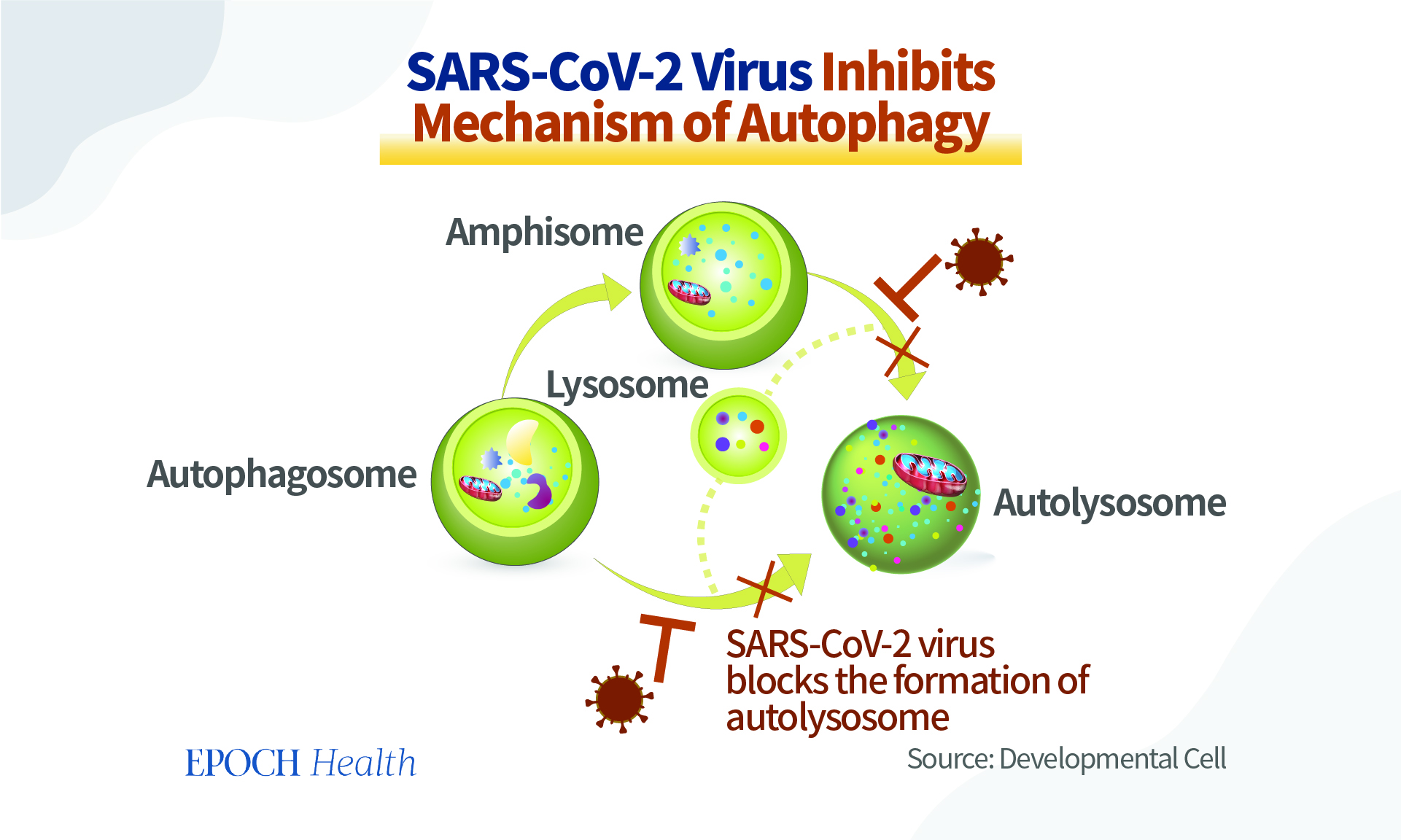
During the process of autophagy, an autophagosome is first produced in the cell, and it acts as a “garbage bag” to wrap the various waste products in the cell. The “garbage bag” will have to fuse with a lysosome (loads of enzymes to break down the garbage) to form a “garbage processing station” called an autolysosome, which will break down and recycle the wrapped waste materials.
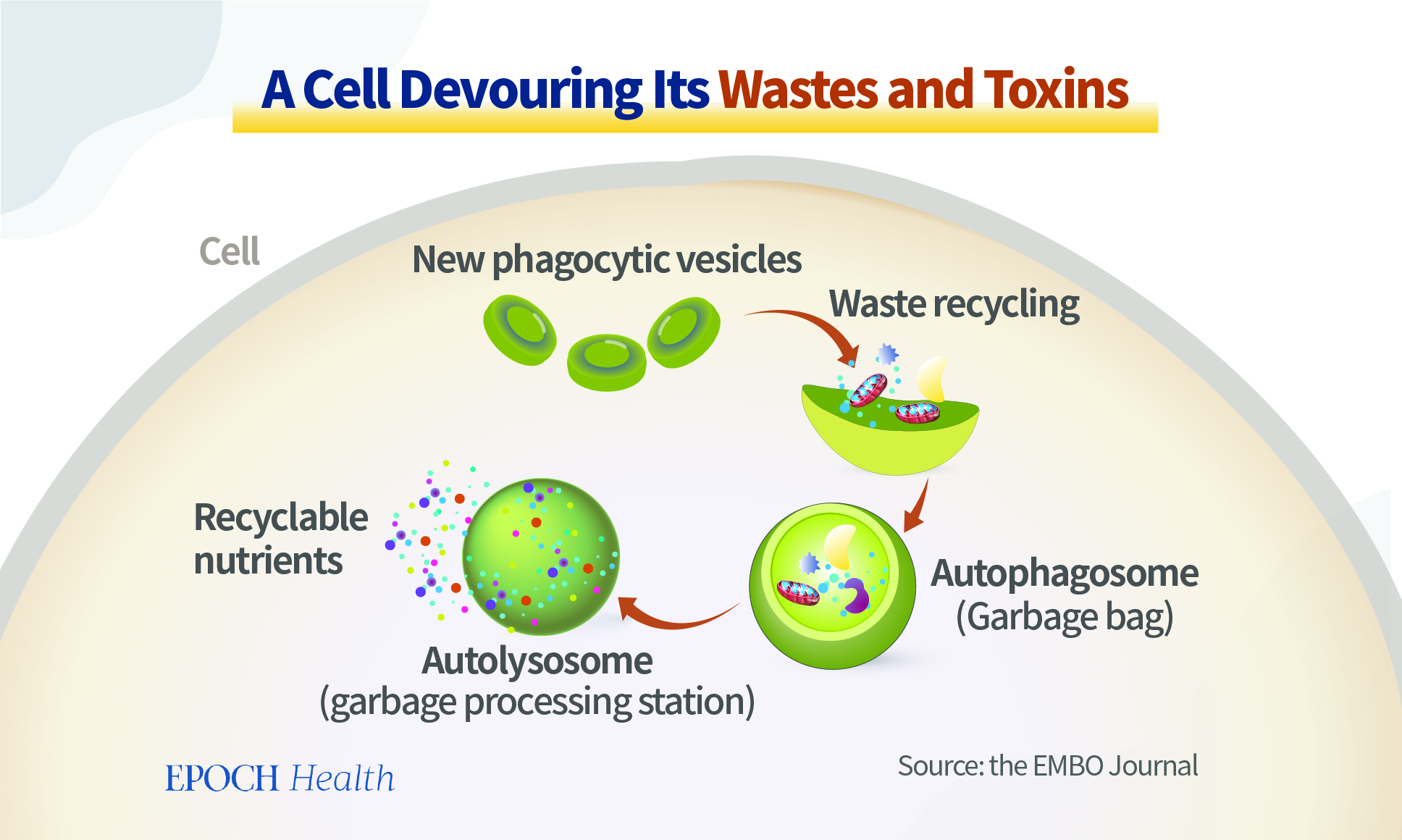
Autophagy is an important physiological mechanism that not only removes harmful components from cells in a timely manner, but also transforms useless proteins into recyclable amino acids. This brings a variety of benefits to the body, including anti-aging benefits, reduced inflammatory status, boosted immunity, and reduced cancer risk.
In cells infected with the SARS-CoV-2 virus, the formation of autolysosomes has been blocked, substantially resulting in many more garbage bags but reduced processing ability. SARS-CoV-2 virus blocks the formation of autolysosomes, and prevents the timely recycling of waste and harmful substances in the cells.
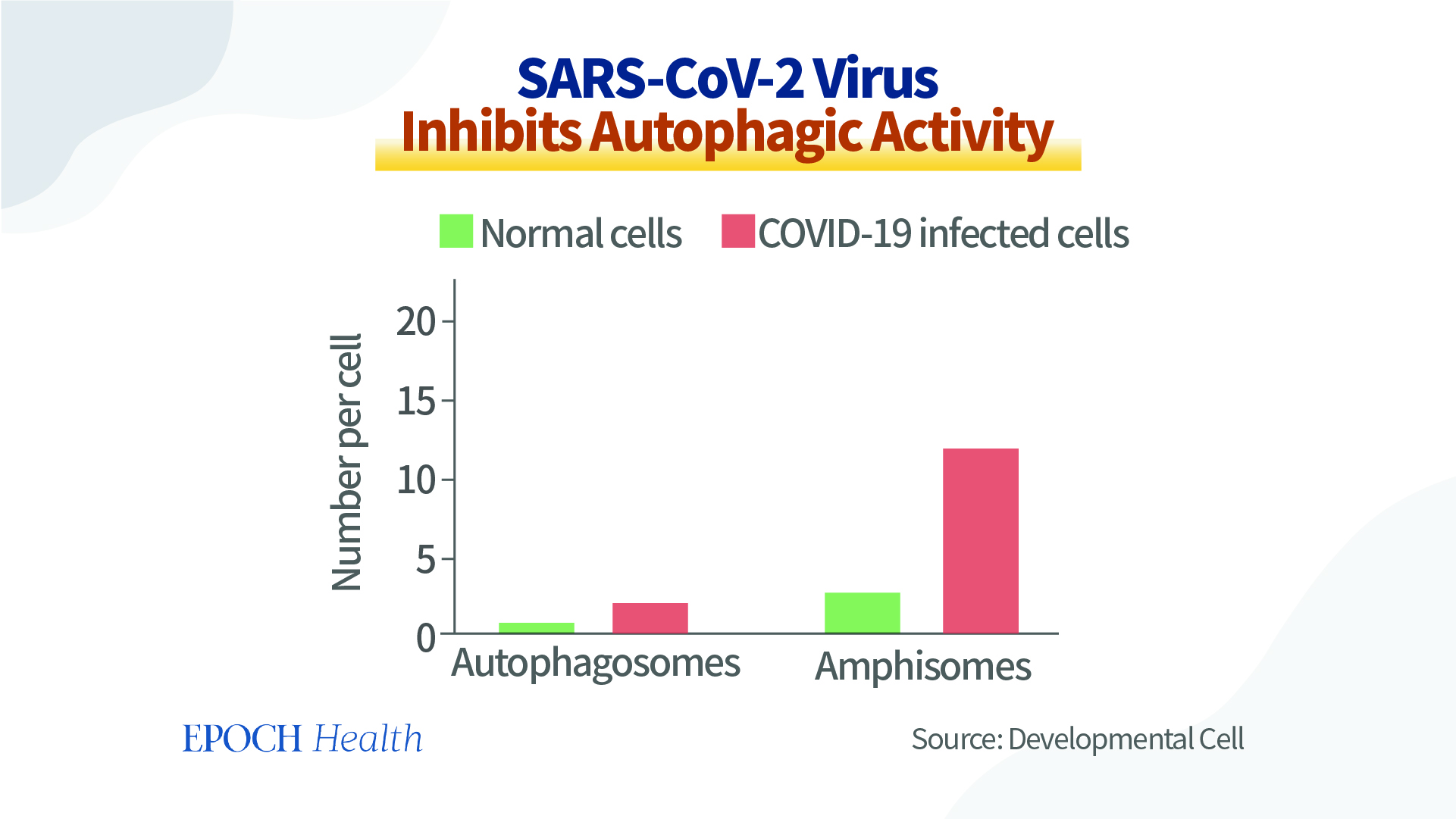
In addition, the inhibition of autophagy leads to the accumulation of undigested viral proteins and genetic material in cells, increasing the secretion of pro-inflammatory factors and causing cytokine storms, which are even worse for the already fragile neuronal cells.
Autophagy dysregulation has many harmful effects on the body, especially on the nervous system. This is because neuronal cells are unlike our skin cells, which renew regularly and when damaged. Neuronal cells have a long life span, and cannot be renewed at any time when they are damaged, so they need to rely on the autophagy system to clean and repair themselves in response to external stressors.
So, neuronal cells are extremely sensitive to such disruptions. Without an effective rescue, one can imagine the impact of such cells being nearly corrupted and dying.
In addition, autophagic activity decreases with age. Therefore, autophagic dysfunction can exacerbate illness in the elderly. A study published in the journal eClinicalMedicine found that COVID-19 patients had a cognitive loss equivalent to 20 years of aging, with a loss of 10 IQ points. We can understand this study data better now.
2 Simple Tips to Activate Autophagy
Autophagy plays a very important role in human health. So how can we activate the inhibited autophagy process?
The body automatically activates autophagy when cells are invaded or damaged by pathogens. In addition, intermittent fasting can also activate the autophagy process, because fasting can cause cells to lack nutrients and enter a state of starvation, which will encourage cells to clean up and recycle waste materials. Therefore, fasting can improve many chronic diseases, including diabetes and rheumatism.
We would like to introduce two other novel ways to effectively activate autophagy.
1. Terpene Nutrients
Plants provide us with many health-improving nutrients.
In an article published in the journal Aging in 2021, Russian scientists mentioned that terpenes extracted from Siberian fir trees could effectively activate autophagy.
After treating cells with terpenes for 24 hours, the percentage of cells containing autophagosomes (garbage bags) or autophagolysosomes (garbage processing stations) both increased significantly compared to the control group, and the number of autophagosomes contained in a single cell also increased.
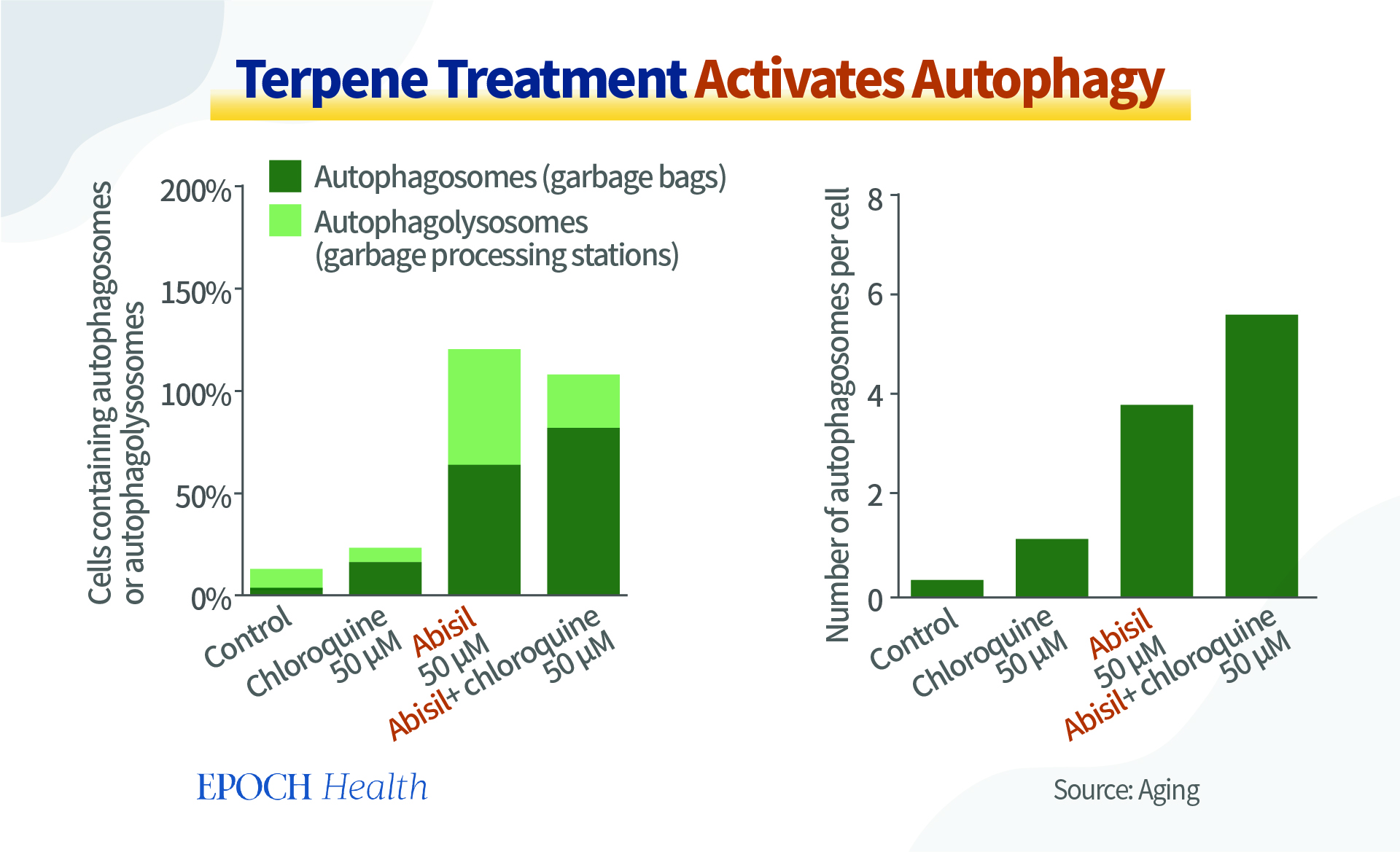
Terpenoids are the main components of many plant essential oils. Essential oils are also widely used in aromatherapy. For instance, citrus peel and peppermint essential oil can help improve mood and spirit.
According to statistics, the total number of known terpenoids exceeds 22,000, and they are one of the most important sources for the development of new therapies.
2. Sitting in Meditation
Another therapy that can activate autophagy is sitting in meditation.
A study published in the journal Nature – Translational Psychiatry in 2016 observed 64 healthy women, half of whom were given a vacation while the other half meditated.
After one week, it was found that the meditators had significantly lower serum Aβ40, which implies increased autophagy in brain nerve cells and a reduced risk of dementia.
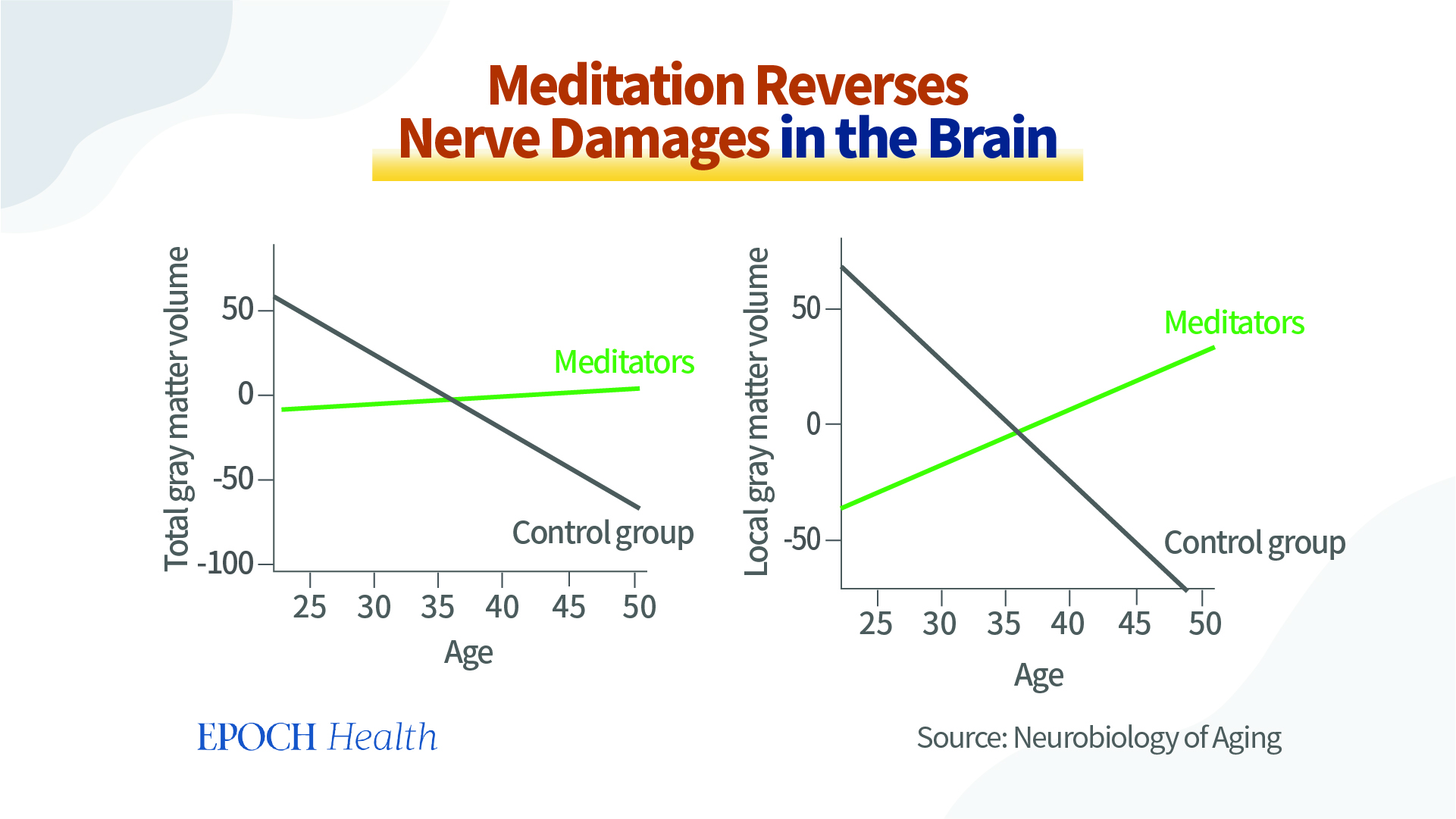
This finding echoes the findings of a study published in the journal Neurobiology of Aging in 2007.
The study compared the gray matter volume in the brains of meditators and non-meditators. It was discovered that the gray matter volume of the meditators did not shrink with age, but even increased, suggesting that meditation reverses the aging of and damage to the brain.
Meditators also showed great improvement in the ability to concentrate and in their response times, which may help long COVID patients suffering from brain fog.
This prolonged pandemic has affected the human body in many ways, including putting tremendous stress on our neurological and mental health. By taking a holistic approach and understanding the close connections between man and nature, the mind and body, we may have a better chance to lift our physical and mental health levels fundamentally.
Reference
https://academic.oup.com/jid/advance-article/doi/10.1093/infdis/jiac136/6569364
https://www.science.org/doi/pdf/10.1126/science.ada0536
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7535629/
https://www.nature.com/articles/s41467-022-29440-z
https://www.nature.com/articles/s41422-020-0390-x
https://www.nature.com/articles/d41586-021-01693-6
https://www.theepochtimes.com/why-long-covid-and-vaccine-injuries-look-so-similar-expert-explains_4665260.html
https://www.cell.com/developmental-cell/fulltext/S1534-5807(20)31016-9
https://journals.lww.com/nrronline/pages/default.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9048584/
https://www.aging-us.com/article/203448/text
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6523335/
https://www.nature.com/articles/tp2016164#MOESM46
https://pubmed.ncbi.nlm.nih.gov/17655980/
No comments:
Post a Comment